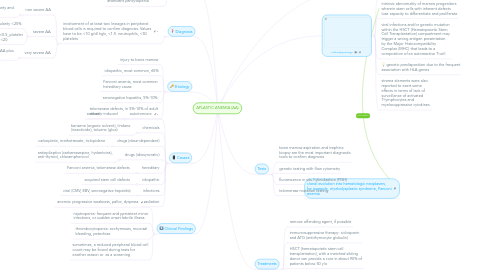
1. Definition
1.1. refers to the syndrome of chronic primary hematopoietic failure from injury leading to diminished or absent hematopoietic precursors in the bone marrow and attendant pancytopenia
2. Diagnosis
2.1. involvement of at least two lineages in peripheral blood cells is required to confirm diagnosis. Values have to be <10 g/dl hgb, <1.5 neutrophils, <50 platelets
2.1.1. non severe AA
2.1.1.1. decreased bone marrow cellularity and peripheral blood cytopenia
2.1.2. severe AA
2.1.2.1. bone marrow cellularity <25%
2.1.2.2. at least 2 of neutrophil count <0.5, platelet count <20, reticulocyte count <20
2.1.3. very severe AA
2.1.3.1. fulfilling criteria of severe AA plus neutrophil count <0.2
3. Etiology
3.1. injury to bone marrow
3.2. idiopathic, most common, 65%
3.3. Fanconi anemia, most common hereditary cause
3.4. seronegative hepatitis, 5%-10%
3.5. telomerase defects, in 5%-10% of adult onset
4. Causes
4.1. autoimmune
4.1.1. antibody-induced
4.2. chemicals
4.2.1. benzene (organic solvent), lindane (insecticide), toluene (glue)
4.3. drugs (dose-dependent)
4.3.1. carboplatin, methotrexate, ticlopidene
4.4. drugs (idiosyncratic)
4.4.1. antiepileptics (carbamazepine, hydantoins), anti-thyroid, chloramphenicol
4.5. hereditary
4.5.1. Fanconi anemia, telomerase defects
4.6. idiopathic
4.6.1. acquired stem cell defects
4.7. infections
4.7.1. viral (CMV, EBV, seronegative hepatitis)
4.8. radiation
5. Clinical Findings
5.1. anemia: progressive weakness, pallor, dyspnea
5.2. neutropenia: frequent and persistent minor infections, or sudden onset febrile illness
5.3. thrombocytopenia: ecchymoses, mucosal bleeding, petechiae
5.4. sometimes, a reduced peripheral blood cell count may be found during tests for another reason or as a screening
6. extrinsic immune-mediated suppression of hematopoietic stem cells
6.1. partial defects in telomeres, the component of DNA intertwined with cell division, lead to premature hematopoietic stem cell exhaustion and marrow aplasia; shortened telomeres are present in cells of half of patients with aplastic anemia
7. Pathophysiology
7.1. damaged hematopoietic stem cells mature into self reactive T-helper cells that release cytokines interferon-gamma and tumor necrosis factor to propagate a cytotoxic cascade to kill and suppress other hematopoietic stem cells
7.2. intrinsic abnormality of marrow progenitors wherein stem cells with inherent defects lose capacity to differentiate and proliferate
7.3. viral infections and/or genetic mutation within the HSCT (Hematopoietic Stem Cell Transplantation) compartment may trigger a wrong antigen presentation by the Major Histocompatibility Complex (MHC) that leads to a composition of an autoreactive T-cell
7.4. genetic predisposition due to the frequent association with HLA genes
7.5. stroma elements were also reported to exert some effects in terms of lack of surveillance of activated T-lymphocytes and myelosuppressive cytokines
8. clonal evolution into hematologic neoplasms, for example, myelodysplastic syndrome, Fanconi anemia
9. Tests
9.1. bone marrow aspiration and trephine biopsy are the most important diagnostic tools to confirm diagnosis
9.2. genetic testing with flow cytometry
9.3. fluorescence in situ hybridization (FISH)
9.4. telomerase mutation testing
10. Treatments
10.1. remove offending agent, if possible
10.2. immunosuppressive therapy: ciclosporin and ATG (antithymocyte globulin)
10.3. HSCT (hematopoietic stem cell transplantation), with a matched sibling donor can provide a cure in about 90% of patients below 50 y/o
10.4. umbilical Cord Blood Transplant (CBT)
10.5. supportive therapy
10.5.1. packed red blood cell transfusion with the aim to improve symptoms
10.5.2. platelet infusion when count drops below 10 or in case of bleeding

