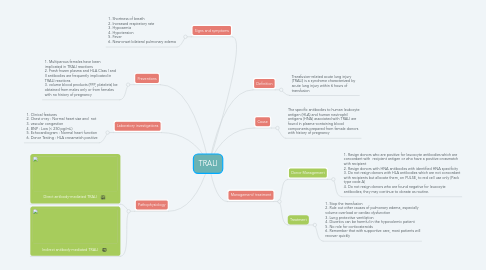
1. Pathophysiology
1.1. Direct antibody-mediated TRALI
1.2. Indirect antibody-mediated TRALI
2. Signs and symptoms
2.1. 1. Shortness of breath 2. Increased respiratory rate 3. Hypoxemia 4. Hypotension 5. Fever 6. New-onset bilateral pulmonary edema
3. Laboratory investigations
3.1. 1. Clinical features 2. Chest x-ray : Normal heart size and not 3. vascular congestion 4. BNP : Low (< 250 pg/mL) 5. Echocardiogram : Normal heart function 6. Donor Testing : HLA crossmatch positive
4. Preventions
4.1. 1. Multiparous females have been implicated in TRALI reactions 2. Fresh frozen plasma and HLA Class I and II antibodies are frequently implicated in TRALI reactions 3. volume blood products (FFP, platelets) be obtained from males only or from females with no history of pregnancy
5. Definition
5.1. Transfusion-related acute lung injury (TRALI) is a syndrome characterized by acute lung injury within 6 hours of transfusion
6. Cause
6.1. The specific antibodies to human leukocyte antigen (HLA) and human neutrophil antigens (HNA) associated with TRALI are found in plasma-containing blood components prepared from female donors with history of pregnancy
7. Management/ treatment
7.1. Donor Management
7.1.1. 1. Resign donors who are positive for leucocyte antibodies which are concordant with recipient antigen or who have a positive crossmatch with recipient 2. Resign donors with HNA antibodies with identified HNA specificity 3. Do not resign donors with HLA antibodies which are not concordant with recipients but allocate them, on PULSE, to red cell use only (Pack type code A) 4. Do not resign donors who are found negative for leucocyte antibodies; they may continue to donate as routine.
7.2. Treatment
7.2.1. 1. Stop the transfusion 2. Rule out other causes of pulmonary edema, especially volume overload or cardiac dysfunction 3. Lung protective ventilation 4. Diuretics can be harmful in the hypovolemic patient 5. No role for corticosteroids 6. Remember that with supportive care, most patients will recover quickly
