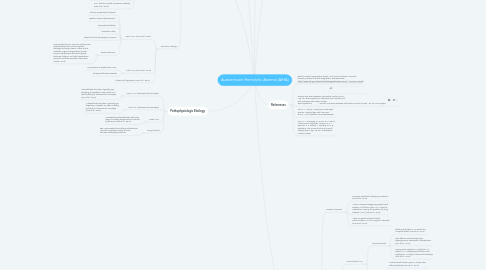
1. Pathophysiologic Etiology
1.1. Warm AIHA (extravascular hemolysis)
1.1.1. Autoantibody formation, typically IgG targeting Rh peptide or RBC band 3 on RBCs leading to extravascular hemolysis (Hue et al., 2016).
1.2. Cold AIHA (intravascular hemolysis)
1.2.1. Autoantibody formation, typically IgM targeting I-i peptide on RBCs, leading primarily to intravascular hemolysis (Hue et al., 2016).
1.3. Mixed AIHA
1.3.1. Mediated by autoantibodies with wide range if binding temperatures, linked to lymphomas (Hue et al., 2016).
1.4. Drug-induced
1.4.1. RBC opsonization by antidrug antibodies or immune complexes; rarely de novo anti-RBC antibody production.
2. Risk Factors (Hue et al., 2016)
2.1. Malignancy
2.2. Lymphoproliferative disorders
2.3. Infection
2.4. Autoimmune disorders
2.5. CVID
2.6. Medications
2.7. No genetic component in majority of cases
3. Diagnostic tests
3.1. CBC and blood smear
3.1.1. Anemia, +/- mild leukocytosis (Hue et al., 2016).
3.1.2. Blood smear examination: anisocytosis, polychromasia (reticulocytotic), macrocytosis (Hue et al., 2016).
3.1.3. Warm AIHA-specific: spherocytes (Hue et al., 2016).
3.1.4. Cold AIHA-specific: agglutinated RBCs (Hue et al., 2016).
3.2. Hemolytic workup
3.2.1. Reticulocyte count, elevated lactate dehydrogenase (LDH), decreased haptoglobin (Hue et al., 2016).
3.2.2. Bilirubinemia: unconjugated (indirect) but can be conjugated (direct) in extravascular hemolysis (Hue et al., 2016).
3.2.3. Hemoglobinuria in cases of intravascular hemolysis (e.g., PCH) (Hue et al., 2016).
3.3. Gold standards: direct antiglobin test (DAT), also known as the Coombs reaction
3.3.1. Warm AIHA: DAT + for IgG +/- C3d (Hue et al., 2016).
3.3.2. Cold AIHA: DAT + for C3d alone, although weak IgG signal in 20% of cases (Hue et al., 2016).
3.3.2.1. Confirmatory test: cold agglutinin titers (with incubation at 4 degrees Celsius) at least 1:64 (Hue et al., 2016).
3.3.3. C3d: Also known as the Anti-Human Globulin Anti-IgG is a direct antiglobulin test to determine the presence of in-vivo coating of red blood cells with antibody molecules and/or complement components (like autoantibodies, maternal antibodies in hemolytic disease of the newborn, and alloantibodies against red blood cells in transfusion reactions) (Biotest Medical Diagnostics, 2008).
3.3.4. Mixed AIHA: DAT + for IgG and C3d (Hue et al., 2016).
3.3.5. PCH: test for Donath-Lansteiner antibody (Hue et al., 2016).
3.4. Common Findings
3.4.1. Warm AIHA (Hue et al., 2016)
3.4.1.1. Chronic lymphocytic leukemia
3.4.1.2. Systemic lupus erythematosus
3.4.1.3. Rheumatoid arthritis
3.4.1.4. Ulcerative colitis
3.4.1.5. idiopathic thrombocytopenic purpura
3.4.1.6. Evans syndrome
3.4.1.6.1. Evans syndrome is a very rare autoimmune disorder where the immune system destroys the body's RBCs, WBCs and/or platelets. Signs and symptoms include purpura (red/purple discolored spots), paleness, fatigue, and light-headedness (Genetic and Rare Diseases Information Center, 2016).
3.4.2. Cold AIHA (Hue et al., 2016)
3.4.2.1. Mycoplasma or Epstein-Barr virus
3.4.2.2. lymphoproliferative disease
3.4.3. Plasma cell dyscrasias (Hue et al., 2016)
4. Causative Factors
4.1. Classified in to 3 groups
4.1.1. Warm AIHA (antibodies optimally bind at 37°C): IgG-mediated; triggers are idiopathic or secondary to a triggering process (Hue et al., 2016).
4.1.2. Cold AIHA (antibodies optimally bind at 4-18°C): Usually, IgM-mediated (however, could be instigated by IgA or IgG) includes cold agglutinin (a substance that causes particles to coagulate) syndrome and paroxysmal cold hemoglobinuria (Hue et al., 2016).
4.1.3. Mixed AIHA (antibodies bind from 4-37°C): Primarily IgM-mediated related to lymphomas; displays features of both warm and cold AIHA (Hue et al., 2016).
4.2. Drug-induced AIHA: associated with drug exposure, works similarly to warm AIHA (mainly IgG-mediated) (Hue, Banerjee, & Lau, 2016).
5. Treatments
5.1. General Measures
5.1.1. Treat any identified underlying conditions (Hue et al., 2016).
5.1.2. Avoid or suspend triggering agents (cold weather or fluids for cold AIHA, stop the medication causing the problem for drug induced AIHA) (Hue et al., 2016).
5.1.3. Vitamin supplementation (folate, calcium/vitamin D if on long-term steroids) (Hue et al., 2016).
5.2. Medications
5.2.1. Warm/mixed AIHA
5.2.1.1. Glucocorticoids
5.2.1.1.1. Effective but takes 3-13 months for complete effect (Hue et al., 2016).
5.2.1.1.2. Side effects include weight gain, hyperglycemia, depression, osteoporosis (Hue et al., 2016).
5.2.1.1.3. Dosing oral prednisone 1mg/kg for 3-4 weeks, or IV methylpnisolone 250-1000 mg/day for 1-3 days if continued hemolysis (Hue et al., 2016).
5.2.1.2. Danazol
5.2.1.2.1. Most successful when given in conjunction with prednisone (Hue et al., 2016).
5.2.1.2.2. Black-box warning in pregnancy, androgenic side effects in women (Hue et al., 2016).
5.2.1.2.3. Long-term hepatotoxicity risk (Hue et al., 2016).
5.2.1.2.4. Dosing 400-800 mg PO daily (Hue et al., 2016).
5.2.2. Cold AIHA
5.2.2.1. Glucocorticoids have low efficacy
5.2.2.2. Rituximab
5.2.2.2.1. Partial response in 54-58% of people (Hue et al., 2016).
5.2.2.2.2. Side effects are uncommon but include hypotension, fever, infection(Hue et al., 2016).
5.2.2.2.3. Dosing 375 mg/m² IV infusion repeated periodically (Hue et al., 2016).
5.2.2.3. Fludarabine
5.2.2.3.1. Synergistic with rituximab but higher immunosuppression risk when used simultaneously (Hue et al., 2016).
5.3. Surgery/Other procedures
5.3.1. RBC transfusion
5.3.1.1. Supportive measures to improve oxygenation; minimize transfusion amount when feasible (Hue et al., 2016).
5.3.1.2. Warm AIHA
5.3.1.2.1. Urgent setting: Transfuse with typed and crossed blood. There is a 33% chance of worsening hemolysis due to alloantibodies to minor RBC antigens (Hue et al., 2016).
5.3.1.2.2. Nonurgent setting: extended RBC pretransfusion workup, including RBC phenotyping and antibody detection (Hue et al., 2016).
5.3.1.3. Cold AIHA
5.3.1.3.1. Typed and crossed blood transfusion; additonal testing generally not required (Hue et al., 2016).
5.3.1.3.2. All RBC compatibility tests should be completed at 37°C (Hue et al., 2016).
5.3.1.3.3. Use prewarmed blood products to avoid hemolytic crisis (Hue et al., 2016).
5.3.2. Splenectomy
5.3.2.1. 38-70% success rate in warm/mixed AIHA (Hue et al., 2016).
5.3.2.2. Not effective in cold AIHA (Hue et al., 2016).
5.3.2.3. Splenectomy not recommended in pediatrics given typically self-limited course (Hue et al., 2016).
5.3.2.4. Vaccine ALERT
5.3.2.4.1. Vaccinate against encapsulated bacteria (streptococcus pneumoniae, Neisseria meningitidis, Haemophilus influenzae) at minimum of 2 weeks before splenectomy (Hue et al., 2016).

