1. Diagnostic Tests
1.1. Spirometry Test
1.2. Pulmonary function testing
1.3. Vital Capacity
1.4. Arterial blood gas test
2. Risk Factors
2.1. Age
2.2. mostly in Male gender
2.3. Reduced lung function
2.4. Air pollution
2.5. Exposure to second hand smoke or smokers
2.6. Familial allergies
2.7. Poor nutrition
2.8. Alcohol intake
2.8.1. 2x higher in men between 65-74
2.8.2. 3x higher in men between 75-84
3. Signs and Symptoms
3.1. Chronic and Progressive dyspnea
3.2. Coughing and wheezing
3.2.1. Shortness of Breath
3.3. Sputum production
3.4. Chest tightness
3.5. Other signs may be: weight loss, anorexia, depression, and anxiety
4. Medical Treatment
4.1. Pharmacotherapy
4.2. Regular exercise
4.3. Phosphodiesterase- 4 inhibitors
4.4. Quit smoking
4.5. Oxygen therapy
4.6. Medication: Bronchodilator, Steroid
4.7. Others: Rescue inhalers and inhaled or oral steroids that help control symptoms and decrease further damage
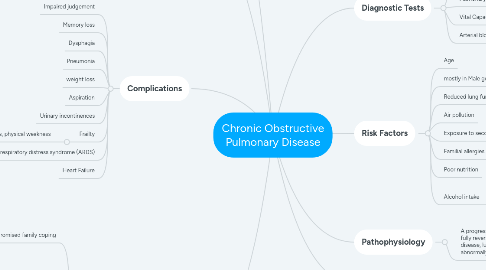
5. Complications
5.1. Impaired judgement
5.2. Memory loss
5.3. Dysphagia
5.4. Pneumonia
5.5. weight loss
5.6. Aspiration
5.7. Urinary incontinences
5.8. Frailty
5.8.1. Risk for falls, physical weakness
5.9. Acute respiratory distress syndrome (ARDS)
5.10. Heart Failure
6. Pathophysiology
6.1. A progressive airflow limitation that is not fully reversible and during the course of the disease, lung tissue that becomes abnormally inflamed
7. Nursing Diagnosis/ Nursing Interventions
7.1. Compromised family coping
7.1.1. Establishing an effective communication system with the patient and his family to help them adjust to the patients altered cognitive abilities
7.1.2. Provide emotional support to the patient and his family
7.1.3. Encourage the family to allow the patient as much independence as possible while ensuring safety to the patient and others
7.2. Impaired physical mobility/ powerlessness/ Imbalanced nutrition
7.2.1. Provide rest periods between activities because the patient tires easily
7.2.2. Encourage the patient independence and allow ample time for patient to perform task
7.2.3. Encourage sufficient fluid intake and adequate nutrition
7.2.4. Monitor patients fluid intake detect imbalances
7.3. Risk for infection
7.3.1. Monitor Temperature
7.3.2. Observe color charter and odor of sputum
7.3.3. Monitor Visitors; provide masks as needed
7.4. Ineffective airway clearance
7.4.1. Check vital signs
7.4.1.1. Auscultate breath sounds
7.4.2. Assume a position of comfort
7.4.2.1. Elevate the head of the bed
7.4.3. Keep environment pollution free such as dust and smoke
7.4.4. Observe characteristics of coughing

