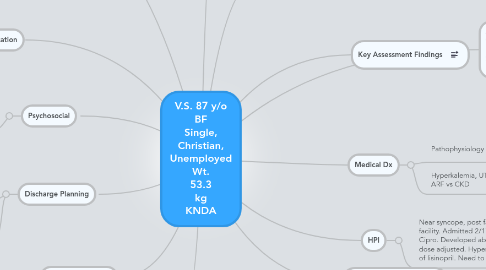
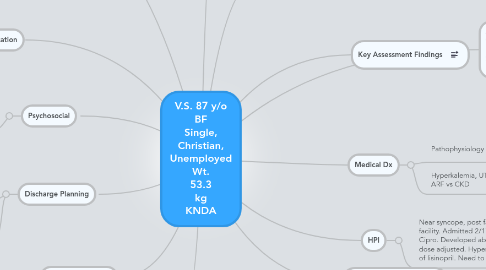
V.S. 87 y/o BF Single, Christian, Unemployed Wt. 53.3 kg KNDA
저자: Melissa Ivester
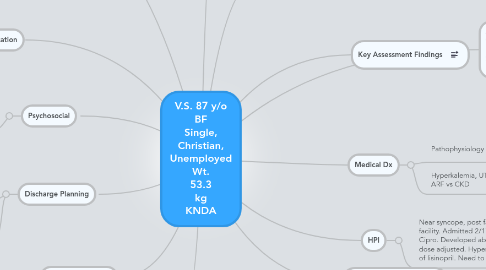
1. Discharge Planning
1.1. Rule out CKD vs ARF. If it is determined that there is a need for dialysis, would need to get social work involved to connect her with a dialysis facility. Insure resources and support is available.
1.2. Labs showed elevated TSH and T4 values. Follow-up in 12 mth (per doctor) to monitor for hypothyroidism.
2. Goals
2.1. Nursing Intervention1
2.1.1. Monitor lab values (Bun, Cr, serum electrolytes, glucose, and ABGs).
2.1.1.1. Outcome
2.1.1.2. Rationale
2.2. Nursing intervention 2
2.2.1. Assess extent of impairment in thinking ability, memory, and orientation.Note behavior changes, increased stupor/somnolence.
2.2.1.1. Outcome
2.2.1.2. Rationale
3. Priority Nursing Dx
3.1. Risk for disturbed Thought Processes r/t accumulation of toxins (urea, ammonia), metabolic acidosis, hypoxia, electrolyte imbalance, calcifications in the brain.
4. Psychosocial
4.1. Hx of dimentia. Lives at an assisted living facility. No family or relatives for support.
5. Pt Education
5.1. Education needed for her caregivers on a renal diet including fluid restriction, low sodium and low phosphorus. Life style changes associated with dialysis.
6. Medications: Amlodipine 10mg PO Daily Aspirin 81mg PO Daily Atenolol 25mg PO Daily Ciproflaxacin 250 mg in 1L D5W IV Ciproflaxacin 25mg PO for 3 days HydrALAZINE25mg PO q8H Lisonpril 40mg PO Daily Acetametophin 650mg PRN for pain Bisacodyl 10mg PRN for constipation NS .9% 1000mL DC 2/21/12
7. A&Ox2 to person and place (norm for pt). Pupils PERRLA. 99% on RA, diminished lung sounds in LLQ and RLQ. No wheezing or other adventitious lung sounds. NSR with first degree AV block. No murmurs/thrils, +2 peripherl pulses, no edema. Skin intact, cool, no masses or redness. Mucus membranes pink and moist. Urine is yellow, clear, odorless. Bowel Sounds normoactive all 4 quadrants. Last BM 2/18/12 (3 days prior).
8. Management
8.1. Complications
9. Key Assessment Findings
10. Diagnostics
10.1. New node
11. Risk Factors
11.1. PMH: HTN, Dyslipidemia, DM, Dimentia
12. Medical Dx
12.1. Pathophysiology
12.2. Hyperkalemia, UTI ARF vs CKD
13. HPI
13.1. Near syncope, post fall from an assisted living facility. Admitted 2/17/12. Treated for UTI with Cipro. Developed abnormal kidney lab values, dose adjusted. Hyperkalemia resolved by D/C of lisinopril. Need to rule out CKD vs ARF.