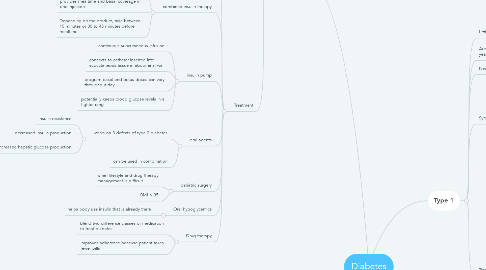
1. Type 2
1.1. Cells don't respond to insulin (resistant), pancreas can't produce greater insulin levels needed of the resistance.
1.1.1. Delay or insufficient insulin secretion
1.1.1.1. increased insulin demand
1.1.1.1.1. B cell exhaustion
1.2. Risk factors: Overweight, obesity, advanced age, family history
1.3. Generally affects people under the age of 40. Has a gradual onset and can have for years without symptoms.
1.3.1. Greater prevalence in ethnic groups
1.4. Genetic link
1.4.1. 1. insulin resistance
1.4.1.1. 2. decrease insulin production
1.4.1.1.1. 3. inappropriate septic glucose production
1.5. Symptoms
1.5.1. Urinating often
1.5.2. being thirsty more than usual
1.5.3. being hungry more often than usual
1.5.4. being more tired than usual
1.5.5. irritability
1.5.6. blurry vision
1.5.7. wounds that won't heal
1.5.8. numbness or tingling in hands or feet
1.6. Conforming diagnosis
1.6.1. Fasting plasma glucose
1.6.1.1. 126 mg/dL or higher on two separate occasions
1.6.2. HbA1c
1.6.2.1. 6.5% or higher on 2 separate occasions
1.6.3. Oral glucose tolerance (OGTT)
1.6.3.1. 2- hour post OGTT blood glucose 200 mg/dL or higher
1.7. Treatment
1.7.1. Exogenous insulin
1.7.1.1. prescribed for patients who cannot manage blood glucose levels by other means
1.7.2. combined insulin therapy
1.7.2.1. short acting or rapid acting insulin with intermediate acting insulin in same syringe
1.7.2.2. provides mealtime and basal coverage in one injection
1.7.2.3. Depending on the product, take between 10 minutes or 30 to 45 minutes before mealtime
1.7.3. insulin pump
1.7.3.1. continuous subcutaneous infusion
1.7.3.2. connects to catheter inserted into subcutaneous tissue in abdominal wall
1.7.3.3. program basal and bolus doses can vary throughout day
1.7.3.4. potentially keeps blood glucose levels in a tighter rang
1.7.4. oral agents
1.7.4.1. works on 3 defects of type 2 diabetes
1.7.4.1.1. insulin resistance
1.7.4.1.2. decreased insulin production
1.7.4.1.3. increased hepatic glucose production
1.7.4.2. can be used in combination
1.7.5. bariatric surgery
1.7.5.1. when lifestyle and drug therapy management is difficult
1.7.5.2. BMI > 35
1.7.6. Oral hypoglycemics
1.7.6.1. helps body use insulin that is already there
1.7.7. Drug therapy
1.7.7.1. blend two difference classes of medication to treat diabetes
1.7.7.2. improves adherence because patient takes fewer pills
2. Insulins
2.1. Rapid acting
2.1.1. onset: 10-30 min
2.1.2. peak: 30 min- 3 hr
2.1.3. duration: 3-5 hr
2.1.4. use 15 min before meal time
2.2. short acting
2.2.1. onset: 30 min- 1 hr
2.2.2. peak: 2-5 hr
2.2.3. duration: 5-8hr
2.2.4. use 30-60 min before a meal
2.3. intermediate acting
2.3.1. onset: 1.5-4hr
2.3.2. peak: 4-12hr
2.3.3. duration: 12-18hr
2.4. long acting
2.4.1. onset: 0.8-4hr
2.4.2. peak: less defined or no pronounced peak
2.4.3. duration: 16-24hr
2.5. inhaled insulin
2.5.1. onset: 12-15min
2.5.2. peak: 60 min
2.5.3. duration: 2.5-3 hr
3. Classes of diabetes by lab values
3.1. Fasting glucose (mg/dL)
3.1.1. Normal: <100
3.1.2. Prediabetes: 100-125 (IFG)
3.1.3. Diabetes: > or equal to 126
3.2. 2-h OGTT (mg/dL)
3.2.1. normal: <140
3.2.2. Prediabetes: 140-199 (IGT)
3.2.3. Diabetes: > or equal to 200
3.3. Random Glucose (mg/dL)
3.3.1. normal: <200
3.3.2. Diabetes: > or equal to 200
3.4. A1C
3.4.1. Normal: <5.7%
3.4.2. Prediabetes: 5.7-6.4%
3.4.3. Diabetes: > or equal to 6.5%
4. Type 1
4.1. Little to no insulin is produced
4.1.1. Autoimmune destruction of B cells
4.2. Autoantibodies are present for months to years without symptoms
4.2.1. Manifestations develop when pancreas can no longer produce insulin
4.2.1.1. Rapid onset of ketoacidosis
4.3. Necessitates insulin
4.4. Symptoms
4.4.1. Polyuria
4.4.2. Polydipsia
4.4.3. Polyphagia
4.4.4. Weight loss
4.4.5. Weakness
4.4.6. Fatigue
4.5. Treatment
4.5.1. Exogenous insulin
4.5.1.1. insulin from an outside source
4.5.1.2. required for type 1 diabetes
4.5.2. pancreas transplantation
4.5.2.1. for type 1 diabetes with kidney transplant
4.5.2.2. eliminates need for exogenous insulin, SMBG, dietary restrictions
4.5.3. combination insulin therapy
4.5.3.1. mix short acting or rapid acting and intermediate acting insulin in same syringe
4.5.3.2. provides mealtime and basal coverage in one injection
4.5.4. insulin pump
4.5.4.1. continuous subcutaneous infusion
4.5.4.2. connects to a catheter inserted into subcutaneous tissue in abdominal wall
4.5.4.3. program basal and bolus doses that can vary throughout the day
4.5.4.4. potentially keeps blood glucose levels in a tighter range
4.5.5. drug therapy
4.5.5.1. blend two different classes of medications to treat diabetes
4.5.5.2. improves adherence because patients take fewer pills
5. Prediabetes
5.1. increase risk for developing type 2 diabetes
5.2. impaired glucose tolerance (IGT)
5.2.1. OGTT: 140-199mg/dL
5.3. Impaired fasting glucose (IFG)
5.3.1. Fasting glucose: 100-125 mg/dL
5.4. Intermediate stage between normal glucose homeostasis and diabetes
5.5. Asymptomatic but long term damage is already occurring
5.6. Risk Factors: sedentary, overweight, high BP, age 45+, family history of diabetes, Low HDL
5.7. A1C
5.7.1. used to diagnoses and screen patients with pre diabetes
5.7.2. goal is <6.5% to 7%

