1. Priority Problem 3: anxiety related to difficulty breathing
1.1. Assessment
1.1.1. Observation of physical appearance VS - RR, HR Evaluate sleep patterns
1.2. Intervention
1.2.1. Provide calm, quiet environment Encourage deep, slow breathing Establish & maintain a trusting relationship Use short, simple words
1.3. Client Education
1.3.1. Continue activity gradually & increase as tolerated Discuss S&S of escalating anxiety & ways to interrupt its progression
2. Priority Problem 4: Dehydration due to ineffective fluid intake
2.1. Assessment
2.1.1. Skin turgor, skin colour Eatting patterns Monitor ins & outs CWMS
2.2. Intervention
2.2.1. Assess changes in LOC Record ins & outs Encourage fluid uptake IV fluids if pt unable to take fluids
2.3. Client Education
2.3.1. Discuss health meal & fluid intake Encourage parents to bring client's cup from home for familiarity
3. Total Fluid 1586mL/ 24hr or 64.3mL/hr Urine Output 194.4-218.7mL/ 8hrs
4. Medications
4.1. Salbutamol - bronchodilators - for treatment/ prevention of bronchospasm in asthma - adverse reaction: hyperactivity in children, restlessness, nervousness, chest pain - dosage: 2 puffs q4-6h - assessment: lung sound, pulse, BP
4.2. Flovent - corticosteroids - for maintenance & prophylactic treatment of asthma - Dosage: 88mcg bid - assessment: lung sound, pulse, BP
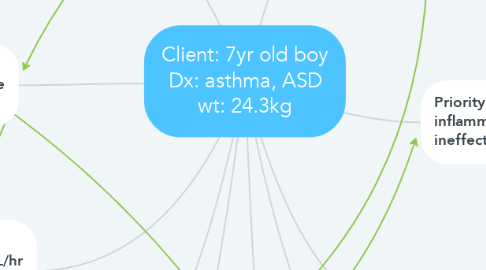
5. Asthma: a chronic inflammatory disease of the airways that causes narrowing & inflammation of the airways and mucus production
5.1. Pathophysiology When the mast cells are activated, it releases mediators such as histamine - hypertrophy of smooth muscle cell -> chest tightness, dyspnea - inflamed/ thickened airway wall - increased mucous production
6. Priority Problem 1: impaired gas exchange related to inefficient delivery of O2
6.1. Assessments
6.1.1. Focused gas exchange assessment - Auscultate lung - S&S of respiratory distress - Skin colour (cyanosis)
6.1.2. VS - RR & depth
6.1.3. Monitor LOC
6.2. Interventions
6.2.1. Monitor O2 sat and administer O2 if required Elevate the head of bed
6.3. Client Education
6.3.1. Explore non-pharmacological methods - Deep breathing - Meditation, quiet environment
7. Priority Problem 2: increased inflammation resulting in ineffective airway clearance
7.1. Assessments
7.1.1. Observe for persistent cough Peak expiratory flow rate using a peak flow meter
7.2. Interventions
7.2.1. Increase fluid intake Administer medications - short-acting beta2 agonist - bronchodilators - leukotriene antagonists Peak flow monitoring
7.3. Client Education
7.3.1. Discussing the asthma action plan Education about the medications and proper usage of a spacer Recognizing and handling worsening asthma Emergency contact information Discussing possible triggers of asthma
