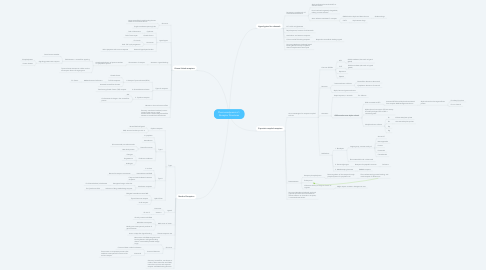
1. Ligand-gated ion channels
1.1. Pentameric complex with 4-5 transmembrane domains
1.1.1. Alpha and beta subunits bind ACh to activate channel
1.1.2. Pore lined with negatively charged AA, making it cation selective
1.1.3. Anion selective mediates Cl- transport
1.1.3.1. GABA binds to alpha and beta subunits
1.1.3.1.1. Sedative drugs
1.1.3.2. 5-HT3
1.1.3.2.1. Psychoactive drugs
1.2. NT = ACh and glutamate
1.3. Rapid response, fractions of milliseconds
1.4. Arachidonic acid sensitive receptors
1.5. Calcium and ATP binding receptors
1.5.1. Respond to intracellular binding signals
1.6. Summary: Membrane localized, ligand binding domain directly coupled to channel complex with central pore
2. G-protein-coupled receptors
2.1. Act as messengers for receptors coupled to them
2.1.1. Common GPCRs:
2.1.1.1. ACh
2.1.1.1.1. Soluble mediator (also work on ligand gated)
2.1.1.2. 5-HT
2.1.1.2.1. Soluble mediator (also work on ligand gated)
2.1.1.3. Dopamine
2.1.1.4. Opiods
2.1.2. Structure:
2.1.2.1. 7 transmembrane a-helices
2.1.2.1.1. Extracellular domain at N-terminal
2.1.2.1.2. Cytoplasmic domain at C-terminal
2.1.2.2. Alpha, beta and gamma subunits
2.1.3. Activation:
2.1.3.1. Rapid response, in seconds
2.1.3.1.1. Ex: olfaction
2.1.3.2. GDP attaches onto alpha subunit
2.1.3.2.1. GDP converted to GTP
2.1.3.2.2. Alpha subunit has intrinsic GTP-ase activity that self-hydrolyses GTP to GDP = inactivating itself
2.1.3.2.3. 20 alpha subunit isoforms
2.1.4. Subfamilies:
2.1.4.1. 1. Rhodopsin
2.1.4.1.1. Largest group, consists mainly of:
2.1.4.1.2. Short extracellular tail in N-terminal
2.1.4.2. 2. Secretin/glucagon
2.1.4.2.1. Receptors for peptide hormones
2.1.4.3. 3. Metabotropic glutamate
2.1.4.3.1. GABAb receptors
2.2. Desensitization
2.2.1. Receptor phosphorylation
2.2.1.1. Down-regulation of the receptor through phosphorylation of cytoplasmic tail
2.2.1.1.1. This interferes with g-protein binding, and marks receptor for destruction
2.2.2. Endocytosis
2.2.3. Influences efficacy of drugs on chronic tx regimen
2.2.3.1. Might require increase in dosage over time
2.3. Summary: Membrane localized, work with g-protein activation that translocates to activate effector ion channels or enzymes; 7 transmembrane helices
3. Kinase-linked receptors
3.1. Structure:
3.1.1. Large extracellular ligand-binding domain linked to intracellular domain
3.1.2. Single membrane spanning helix
3.2. Ligand types:
3.2.1. Cytokines
3.2.1.1. Role: Inflammation
3.2.2. Growth factors
3.2.2.1. Role: Tissue repair
3.2.3. Hormones
3.2.3.1. Ex: Insulin
3.2.3.2. Role: Cell cycle progression
3.2.4. Bacterial lipopolysaccharides
3.2.4.1. Role: Apoptosis and immune response
3.3. Activation: Ligand binding
3.3.1. Dimerization of receptor
3.3.1.1. Autophosphorylation of tyrosine residues on cytoplasmic portion
3.3.1.1.1. SH2 domains = intracellular signaling
3.3.1.1.2. Tyrosine kinase activates or inhibits nuclear transcription factors of target genes
3.4. Types of receptors:
3.4.1. 1. Receptor Tyrosine kinases (RTKs)
3.4.1.1. Growth factors
3.4.1.2. Toll-like receptors
3.4.1.2.1. Mediate bacterial infections
3.4.1.3. Activated intracellular domains
3.4.2. 2. Serine/threonine kinase
3.4.2.1. Transforming Growth Factor (TGF) receptor
3.4.3. 3. Cytokine receptors
3.4.3.1. JAK
3.4.3.2. Conformational change in the intracellular portion
3.5. Minutes or hours to have an effect
3.6. Summary: membrane localized, intrinsic protein kinase activity, single transmembrane helix linking extracellular domain to intracellular kinase domain
4. Nuclear Receptors
4.1. Type:
4.1.1. Orphan receptors
4.1.1.1. No well defined ligand
4.1.1.2. RXR, structural similarity to VIt. A
4.1.2. Type I
4.1.2.1. In cytoplasm
4.1.2.2. Homodimers
4.1.2.3. Steroid hormones
4.1.2.3.1. Glucocorticoids, mineralcorticoids
4.1.2.3.2. Heat shock protein
4.1.2.4. Endocrine mediators
4.1.2.4.1. Estrogen
4.1.2.4.2. Progesterone
4.1.2.4.3. Androgen
4.1.3. Type II
4.1.3.1. In nucleus
4.1.3.2. Heterodimers with RXR
4.1.3.2.1. Retinoid X receptor co-activation
4.1.3.3. Fatty acid and cholesterol sensitive receptors
4.1.3.4. Xenobiotic receptors
4.1.3.4.1. Recognize foreign molecules
4.1.3.4.2. Induction of drug metabolizing enzymes
4.1.4. Hybrid Class
4.1.4.1. Obligate heterodimers were RXR
4.1.4.2. Thyroid hormone receptor
4.1.4.3. Vit D receptor
4.2. Ligand:
4.2.1. Hormones
4.2.2. Vitamins
4.2.2.1. Ex: Vit. D
4.3. Mechanism of action:
4.3.1. Directly interact with DNA
4.3.2. Modulate transcription
4.3.3. Mostly post-transcriptional products of gene activation
4.4. Slowest response rate
4.4.1. Hours or days after ligand binding
4.5. Structure:
4.5.1. Monomeric with DNA recognition and binding domain and ligand binding domain connected by flexible linkage hinge
4.5.2. 2 terminal domains
4.5.2.1. C-terminal does nuclear localization
4.5.2.2. N terminal
4.5.2.2.1. Co-activator or co-repressor proteins that modulate transcriptional functions of the nuclear receptor
