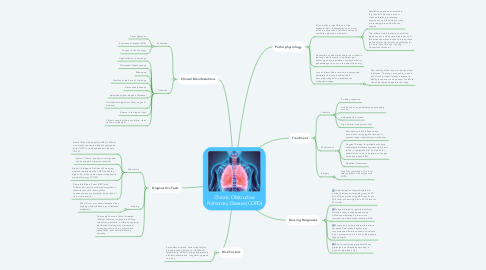
1. Risk Factors
1.1. Secondhand smoke, factors that affect growth during gestation or childhood (prematurity, asthma), airway hyperactivity, alcohol consumption, long-term cigarette smoking
2. Clinical Manifestations
2.1. Subjective
2.1.1. Chest tightness
2.1.2. Shortness of breath (SOB)
2.1.3. Fatigue (lack of energy)
2.2. Objective
2.2.1. Hyperinflation of the lungs
2.2.2. Decreased breath sounds
2.2.3. Wheezing
2.2.4. Crackles at the base of the lungs
2.2.5. Distant heart sounds
2.2.6. Barrel chest (later stages of disease)
2.2.7. Unintended weight loss (later stages of disease)
2.2.8. Edema in the legs or feet
2.2.9. Chronic cough with mucus (white, clear, yellow or greenish)
3. Diagnostics Tests
3.1. Laboratory
3.1.1. Arterial Blood Gas Analysis (ABG): Mild of moderate hypoxemia without hypercapnia (mild COPD) or with hypercapnia (severe COPD).
3.1.2. Sputum Culture: positive microorganism and neutrophils (chronic bronchitis).
3.1.3. Alpha-1-Antitrypsin Deficiency Screening: positive in patients with COPD under the age of 40, or those who have strong family medical history of COPD.
3.1.4. Complete Blood Count (CBC) with Differential: revel secondary polycythemia (hematocrit and/or hemoglobin concentrations are elevated) indications of chronic bronchitis.
3.2. Imaging
3.2.1. Chest X-ray: may show decreased lung markings, hyperinflation, and flattened diaphrams.
3.3. Pulmonary Function Tests: increased residual volumes, increased total lung capacities, decrease in diffusion capacity, decreased vital capacity, decreased forced expiratory flow, normal static compliance, and normal diffusing capacity.
4. Pathophysiology
4.1. Inflammation of the fibrosis of the bronchial wall + hypersecretion of mucus result in obstruction of airflow and cause ventilation perfusion mismatch.
4.1.1. Ventilation perfusion mismatch is the condition where an area or areas of the lung is receiving oxygen but no blood flow, or they are receiving blood flow but no oxygen.
4.1.2. The inflamed walls become constricted which causes a more narrow pathway and the increased mucus builds up along these walls and also narrows these pathways for the air to travel through, causing obstruction for the air.
4.2. Destruction of alveolar tissue (air sac tissue) in the lungs which results in inefficient gas exchange due to decrease of surface area for gas exchange to occur in the alveoli (air sacs).
4.3. Loss of elastic fibers results in a decreased expiratory flow rate resulting in air becoming trapped and predisposes collapsed airways.
4.3.1. The inability of the lungs to rebound from inhalation. The lungs are unable to push out all the air that it intakes because its ability to rebound is decreased. Therefore the air becomes trapped in the lungs.
5. Nursing Diagnoses
5.1. Impaired gas exchanged related to patient's increased respiratory rate of 30 and SOB as evidence by ABG results of a PO2 level of 40mmHg and a PCO2 level of 65mmHg.
5.2. Fatigue related to impaired ability to maintain usual routines evidence by difficulty ambulating 30 feet to the restroom and back without feeling SOB.
5.3. Excess fluid volume related to patients excessive fluid intake beyond their recommended fluid restriction as evidence by 3+ pitting edema in both of the patients legs and feet.
5.4. Risk for ineffective peripheral tissue perfusion as evidence by smoking a pack of cigarettes a day.
6. Treatment
6.1. Lifestyle
6.1.1. Smoking cessation
6.1.2. Avoidance of air pollutants and secondary smoke
6.1.3. Adequate fluid intake
6.1.4. High calorie, high protein diet
6.2. Medications
6.2.1. Vaccinations: both influenza and pneumococcal conjugate vaccines to prevent further respiratory complications.
6.2.2. Oxygen Therapy: for patients who have coexisting pulmonary hypertension, heart failure, or polycythemia. As well as for patients who can not maintain an oxygen saturation above 88%.
6.2.3. Nebulizer Treatments
6.3. Surgery
6.3.1. Lung Transplantation: this is for select patients with very severe COPD.
