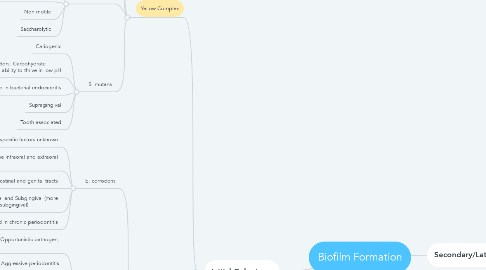
1. Initial Colonizers
1.1. Yellow Complex
1.1.1. S. mitis
1.1.2. S. oralis
1.1.3. S. sanguis
1.1.4. S. gordonii
1.1.5. S. intermedius
1.1.5.1. Virulence factors: Hyaluronidase, Cytotoxins
1.1.5.2. Present in normal oral flora, also known to occur in abscesses
1.1.5.3. Non-motile
1.1.5.4. Saccharolytic
1.1.6. S. mutans
1.1.6.1. Cariogenic
1.1.6.2. Virulence factors: Carbohydrate metabolism, ability to thrive in low pH
1.1.6.3. Indicated in bacterial endocarditis
1.1.6.4. Supragingival
1.1.6.5. Tooth associated
1.2. Green Complex
1.2.1. E. corrodens
1.2.1.1. Virulence factors: specific factors unknown
1.2.1.2. Known to cause intraoral and extraoral infections
1.2.1.3. Also found in intestinal and genital tracts
1.2.1.4. Supragingival and Subgingival (more prevalent in subgingival)
1.2.1.5. Found in chronic periodontitis
1.2.2. C. gingivalis
1.2.2.1. Virulence factors: Opportunistic pathogen; Tissue invasion
1.2.2.2. Aggressive periodontitis
1.2.2.3. Present in normal oral flora and in periodontal pockets
1.2.2.4. Facultative anaerobe
1.2.3. C. sputigena
1.2.4. C. ochracea
1.2.5. C. concisus
1.2.6. A. actinomycetecomitans
1.2.6.1. Virulence factors: Production of leukotoxins; Lipopolysaccharides on cell wall; Secretion of cell stress protein
1.2.6.2. Aggressive periodontitis
1.2.6.3. Tissue associated
1.2.6.4. Subgingival - invades CT
1.2.6.5. Can also cause extraoral infections
1.3. Purple Complex
1.3.1. V. parvula
1.3.2. A. odontolyticus
1.4. Actinomyces species
1.4.1. Virulence factors: Opportunistic pathogens; Invades tissue
1.4.2. Present in abscesses and in normal oral flora
1.4.3. Non-motile
1.4.4. Predominantly anaerobic
1.5. Lactobacillus species
1.5.1. Virulence factors: sucrose metabolism
1.5.2. Supragingival
1.5.3. Colonize in the presence of caries, may be present in low levels normally
1.5.4. Some strains exhibit fluoride resistance
2. Secondary/Late Colonizers
2.1. Orange Complex
2.1.1. C. gracilis
2.1.2. C. rectus
2.1.3. S. constellatus
2.1.4. C. showae
2.1.5. E. nodatum
2.1.6. P. intermedia
2.1.6.1. Virulence factors: Invasion of oral epithelial cells; Fimbriae
2.1.6.2. Aggressive periodontitis
2.1.6.3. Refractory periodontitis
2.1.6.4. Peri-implant disease
2.1.6.5. Subgingival
2.1.6.6. Opportunistic pathogen
2.1.7. P. nigrescens
2.1.8. P. micros
2.1.9. F. nuc. vincentii
2.1.10. F. nuc. nucleatum
2.1.10.1. Virulence factors: Adhesion to other bacteria; Production of toxic metabolites
2.1.10.2. Not causative on its own but contributes to periodontal diseases by attaching and supporting the attachment of other organisms
2.1.10.3. "Bridge" bacteria
2.1.10.4. Subgingival
2.1.11. F. nuc. polymorphum
2.1.12. F. periodonticum
2.2. Red Complex
2.2.1. P. gingivalis
2.2.1.1. Virulence factors: Enzymes (hyaluronidase, chondroitin sulfatase) – decrease phagocytosis for invasion, chemotaxis inhibitors; Lipopolysaccharide – Bone resorption, Immunoglobulin proteases; Fimbriae, exopolysaccharide, outer membrane proteins – Adhesion or attachment to host outer membrane; Collagenase, trypsin-like protease, gelatinase – Degradation of plasma protease inhibitors, destruction of periodontal tissue; Aminopeptidase – Degradation of iron transport protein
2.2.1.2. Found in chronic periodontitis
2.2.1.3. Subgingival
2.2.1.4. Obligate anaerobe
2.2.2. T. forsythensis
2.2.2.1. Virulence factors: Enzymes implicated in tissue destruction; Surface-lipoproteins activate host cells to release proinflammatory cytokines and induce cellular apoptosis
2.2.2.2. Gingivitis; chronic and aggressive periodontitis
2.2.2.3. Subgingival
2.2.2.4. Anaerobic
2.2.3. T. denticola
2.2.3.1. Virulence factors: Attachment to proteins of fibroblasts; Cytotoxic effect
2.2.3.2. NUG
2.2.3.3. Subgingival
2.2.3.4. Proteolytic
2.2.3.5. Potential bacterial etiologic agent for oral cancer
