1. Tratamiento Farmacologico
1.1. Diureticos
1.1.1. causa hipopotasemia que incrementa el riesgo de arritmias digitalis; potassium supplements should be given prophylactically.
1.2. Verapamil, diltiazem, captopril, propafenone and amiodarone
1.2.1. increase plasma concentration of digoxin → plasma concentration of digoxin is doubled → toxicity can occur.
1.3. Adrenérgicos
1.3.1. Pueden inducir arritmias (ambas incrementan la automaticidad ectópica)
1.3.2. Drogas atropónicas aumentan la absorción
1.4. Propranolol, verapamil, diltiazem and disopyramide:
1.4.1. may additively depress A-V conduction and oppose positive inotropic action.
1.5. Digoxin
1.5.1. Q
1.5.1.1. Succinylcholine:
1.5.2. can induce arrhythmias in digitalized patients.
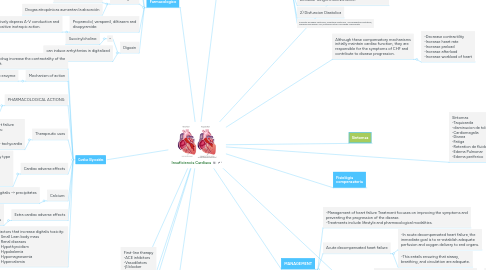
2. Cardiac Glycosides
2.1. This drug increase the contractality of the heart.
2.2. Mechanism of action
2.2.1. Inhibit Na + / K + ATPase enzyme
2.3. PHARMACOLOGICAL ACTIONS:
2.3.1. 1- Increase the force of myocardial contraction (+ve inotropic) leading to decrease in: heart size, venous pressure and edema 2- Slow heart rate ( -ve chronotropic ) by vagal stimulation
2.4. Therapeutic uses
2.4.1. - Congestive heart failure -Atrial arrhythmias: - Atrial flutter - Atrial fibrillation - Supraventricular tachycardia
2.5. Cardiac adverse effects
2.5.1. - digitalis-induced arrhythmias can cause any type of arrhythmia especially: - extrasystoles - coupled beats (Bigeminal rhythms ) - ventricular tachycardia or fibrillation - A.V.block, - cardiac arrest.
2.6. Calcium:
2.6.1. synergises with digitalis → precipitates toxicity.
2.7. Extra cardiac adverse effects
2.7.1. -GIT : common ( the earliest signs of toxicity ): Anorexia,nausea, vomiting, diarrhea CNS: Headache, visual disturbances, drowsiness
2.8. Factors that increase digitalis toxicity: - Small Lean body mass - Renal diseases - Hypothyroidism - Hypokalemia - Hypomagnesemia - Hypercalemia
3. First-line therapy -ACE inhibitors -Vasodilators -β blocker
4. Second-line therapy -Diuretics -Positive Inotropic drugs
5. SEQUENCE-LINE OF THERAPY
6. 2 DISTINCT GOALS OF DRUG THERAPY
6.1. (a) Relief of congestive/low output symptoms: *ACE inhibitors *Vasodilators -nitrate,, nitroprusside,hydralazine *β blocker—Nebivolol, Carvedilol, Metoprolol, bisoprolol *Diuretics—Furosemide (Loop diuretic), thiazides * Positive Inotropic drugs—Digoxin, dobutamine
6.2. (b) Arrest/reversal of disease progression and prolongation of survival: *ACE inhibitors, *β blockers *Aldosterone antagonist- Spironolactone, eplerenone
7. Heart Failure
8. Although these compensatory mechanisms initially maintain cardiac function, they are responsible for the symptoms of CHF and contribute to disease progression.
8.1. -Decrease contractility -Increase heart rate -Increase preload -Increase afterload -Increase workload of heart
9. Síntomas -Taquicardia -disminucion de tolerancia en ejercicio -Cardiomegalia -Disnea -Fatiga -Retention de fluidos -Edema Pulmonar -Edema periferico
10. introducción
10.1. resulta en ventriculo incapaz de llenado completo y disminuye su Fraccion de eyeccion (Aumenta la demanda del trabajo cardiaco.
10.2. Debido a 2 Tipos
10.2.1. Mecanismos Compensatorios: 1)Taquicardia y aumento de contractibilidad atravez del sistema nervioso central. 2)El mecanismo de Frank-Starling 3)Vasoconstriccion 4)Hipertrofia ventricular y deformacion.
10.2.2. 1)Disfunción Sistólica -Reducción en masa muscular, cardiomiopatías, y Hipertrofia Ventricular -Resulta en la incapacidad del ventrículo para bombear sangre efectivamente.
10.2.3. 2) Disfuncion Diastolica
10.2.4. Aumento de rigidez ventricular, Hipertrofia ventricular , Miocardiopatías infiltrativas, isquemia miocardica y IAM, Estenosis Mitral o Tricuspide y pericarditis
11. Síntomas
12. Fisiológia compensatoria
13. MANAGEMENT
13.1. -Management of heart failure Treatment focuses on improving the symptoms and preventing the progression of the disease. -Treatments include lifestyle and pharmacological modalities.
13.2. Acute decompensated heart failure
13.2.1. -In acute decompensated heart failure, the immediate goal is to re-establish adequate perfusion and oxygen delivery to end organs.
13.2.2. -This entails ensuring that airway, breathing, and circulation are adequate.
13.3. Chronic management
13.3.1. -The goals of treatment for people with chronic heart failure are the prolongation of life, the prevention of acute decompensation and the reduction of symptoms, allowing for greater activity.
13.3.1.1. Positive inotropic drugs, very helpful in acute failure. Diastolic dysfunction does not usually respond optimally to positive inotropic drugs
13.3.2. -Treatment strategies provide significant improvement in the relief of symptoms, exercise tolerance, and a decrease in the likelihood of hospitalization or death.
