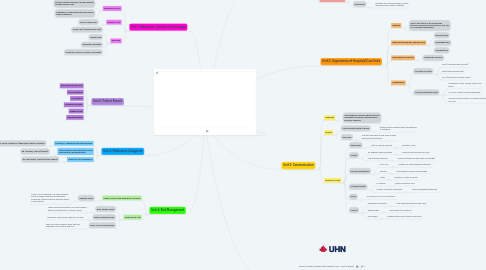
1. Unit 7: Admission, Transfer and Discharge
1.1. Admission Process
1.1.1. Elective: Patients who has a surgery booked for their thoracic area.
1.1.2. Emergency: Unexpected pain that requires medical attention.
1.2. Length of Stay
1.2.1. Four to Seven days.
1.3. Discharge
1.3.1. Home care (Tracheostomy Care)
1.3.2. Oxygen Tank
1.3.3. Respiratory Therapist
1.3.4. Follow-up: Thoracic Surgeon, Oncologist
2. Unit 4: Risk Management
2.1. Safety, Security and Emergency Concerns
2.1.1. Capacity Issues
2.1.1.1. Covid-19 is an example of a surge capacity. Influx of people with serious respiratory conditions at the same time filling up space in the hospital.
2.2. Codes on the Unit
2.2.1. Blue: Cardiac Arrest
2.2.1.1. When doing procedures on or near the heart there is a greater risk for cardiac arrest.
2.2.2. Brown: Hazardous Spill
2.2.2.1. Chemicals used during surgeries may spill.
2.2.3. Grey: Loss of Infrastructure
2.2.3.1. There are many different areas that can experience an infrastructure loss.
3. Unit 5: Medication Categories
3.1. Antibiotics: Substance that fights bacteria.
3.1.1. Eg. Amoxil, Erythrocin (fight against chest infections)
3.2. Anticolinergics: Block the action of the acetylcholine neurotransmitter.
3.2.1. Eg. Atrovent, Spiriva (inhalers)
3.3. Narcotics: Pain medications
3.3.1. Eg. Oxycodone, Tramadol (post surgery)
4. Unit 6: Patient Record
4.1. Pulmonary Function Test
4.2. Echocardiogram
4.3. Consultation
4.4. Discharge Summary
4.5. Imaging Study
4.6. Operative Report
5. .....
6. Unit 1: Health Care Professionals
6.1. Physician(s)
6.1.1. Thoracic Surgeon
6.1.1.1. Surgeon who specializes in treatment pertaining to the heart, lungs and esophagus.
6.1.2. Oncologist
6.1.2.1. Physician who specializes in the treatment and diagnosis of tumours. This physician would be helpful when diagnosing cancer of the thoracic area.
6.2. Consultants
6.2.1. Pulmonologist
6.2.1.1. Physician who specializes in the treatment of the respiratory system.
6.2.2. Cardiologist
6.2.2.1. Physician who specializes in the treatment the cardiovascular system.
6.3. Nursing Staff
6.3.1. Nurse Practitioner
6.3.1.1. Can diagnose, treat and prescribe medication to patients.
6.3.2. Registered Nurse
6.3.2.1. Provide care to patients, monitor and record the patient's health.
6.4. Allied Health Care Workers
6.4.1. Respiratory Therapists
6.4.1.1. Work with patients diagnosed with acute critical respiratory conditions.
6.4.2. Perfusionist
6.4.2.1. Operates the cardiopulmonary bypass machine during cardiac surgeries.
7. Unit 2: Organization of Hospitals/Care Units
7.1. Inpatient
7.1.1. Due to the nature of the procedures typically performed in the Thoracic unit, this is an Inpatient department.
7.2. Diagnoses/Procedures: Thoracic Care
7.2.1. Bronchoscopy
7.2.2. Esophagectomy
7.2.3. Tracheostomy
7.3. Organizational Structure
7.3.1. Therapeutic Services
7.4. Investigations
7.4.1. Common Lab Tests
7.4.1.1. CBC (Complete Blood Count)
7.4.1.2. ABG (Arterial Blood Gas)
7.4.1.3. PFTs (Pulmonary Function Tests)
7.4.2. Common Diagnostic Tests
7.4.2.1. Cardiology: Holter Moniter Tests, EKG, ECHO
7.4.2.2. CT Scans: Chest, Heart/Angiography
7.4.2.3. Nuclear Medicine Tests: Myocardial Perfusion, VQ Scan
8. Unit 3: Communication
8.1. Challenge
8.1.1. Some patients receive surgeries on their esophagus and verbal communication becomes impaired.
8.2. Devices
8.2.1. Communication Book or Board
8.2.1.1. Written communication with a whiteboard or notebook.
8.2.2. Pain Scale
8.2.2.1. Pictures that patients can point to that describe their emotions.
8.3. Direction of Care
8.3.1. Restrictions
8.3.1.1. Quit or reduce smoking
8.3.1.1.1. Healthier Lungs
8.3.2. Activity
8.3.2.1. 45 Degree Fowler's position
8.3.2.1.1. Promote more efficient air flow
8.3.2.2. Low-intensity exercise
8.3.2.2.1. Continue to exercise the lungs for strength
8.3.3. Nursing Interventions
8.3.3.1. PICC Line
8.3.3.1.1. Inserted for chemotherapy treatment
8.3.3.2. Sutures
8.3.3.2.1. Post-surgery sutures and dressings
8.3.3.3. Vitals
8.3.3.3.1. Review O2 Stats and more
8.3.4. IV/Blood/Oxygen
8.3.4.1. IV: Chemo
8.3.4.1.1. Shrink cancerous cells
8.3.4.2. Oxygen: Incentive Spirometer
8.3.4.2.1. Promote breathing exercises
8.3.5. GI/GU
8.3.5.1. No common GI or GU inventions
8.3.6. Consult
8.3.6.1. Respiratory Therapist
8.3.6.1.1. Help with safe exercises and more
8.3.6.2. Respirologist
8.3.6.2.1. Help diagnose conditions
8.3.6.3. Oncologist
8.3.6.3.1. Diagnose cancerous tumours and more

