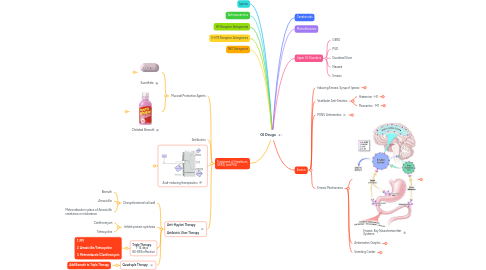
1. Ipecac
2. Antimuscarinics
3. H1-Receptor Antagonists
4. 5-HT3 Receptor Antagonists
5. NK1 Antagonist
6. Treatment of Heartburn, GERD, and PUD
6.1. Mucosal Protective Agents
6.1.1. Sucralfate
6.1.1.1. Treat and Prevent PUD
6.1.1.2. Forms sticky polymer in acidic environment and adheres to ulcer site, forming a barrier
6.1.1.3. Can interfere with other drug absorption
6.1.2. Chelated Bismuth
6.1.2.1. Protects ulcer crater and allows healing
6.1.2.2. Some activity against H. pylori
6.1.2.3. :bangbang: Black Stools, Constipation :bangbang:
6.2. Antibiotics
6.3. Acid-reducing therapeutics
6.3.1. Proton Pump Inhibitors
6.3.1.1. Omeprazole
6.3.1.1.1. **24 hour** prevention of gastric acid release **48 hours** of decreased acid secretion
6.3.2. H2-Receptor Antagonists
6.3.2.1. Slide
6.3.2.2. Cimetidine
6.3.2.3. Famotidine
6.3.2.4. Ranitidine
6.3.2.5. Nizatidine
6.3.3. Antacids
6.3.3.1. Mechanism of Action
6.3.3.1.1. Antacid Neutralizing Capacity (**ANC**)
6.3.3.2. Systemic Antacid
6.3.3.2.1. Sodium Bicarbonate
6.3.3.3. Nonsystemic Antacid
6.3.3.3.1. (**Maalox**) Aluminum Hydroxide + (**Mylanta**) Magnesium Hydroxide Combinations
6.3.3.3.2. (**Tums**) Calcium Carbonate
6.3.3.4. Contraindications
6.3.3.4.1. **Tums** May cause constipation
6.3.3.4.2. **Maalox / Mylanta** are contraindicated in patients with **impaired renal function**
6.3.4. Anticholinergics
6.3.4.1. Pirenzipine
6.3.4.1.1. Muscarinic M1 ACh-R Antagonist
6.3.4.1.2. Blocks gastric acid secretions
6.3.4.1.3. Anticholinergic Side Effects
6.3.5. Prostaglandins
6.3.5.1. Misoprostol
6.3.5.1.1. Decreased gastric acid release
6.3.5.1.2. Stimulates prostaglandin GPCR-inhibitory pathway
6.3.5.1.3. NSAID-induced injury
6.3.5.1.4. Contraindications
6.3.5.1.5. Side Effects
6.4. Anti-H.pylori Therapy Antibiotic Ulcer Therapy
6.4.1. Disrupt bacterial cell wall
6.4.1.1. Bismuth
6.4.1.2. Amoxicillin
6.4.1.3. Metronidazole in place of Amoxicillin resistance or intolerance
6.4.2. Inihibit protein synthesis
6.4.2.1. Clarithromycin
6.4.2.2. Tetracycline
6.4.3. **Triple Therapy**: 7-14 days 80-85% effective
6.4.3.1. 1. PPI 2. Amoxicillin/Tetracycline 3. Metronidazole/Clarithromycin
6.4.4. **Quadruple Therapy**:
6.4.4.1. Add Bismuth to Triple Therapy
7. Canabinoids
8. Phenothiozines
9. Upper GI Disorders
9.1. GERD
9.2. PUD
9.3. Duodenal Ulcer
9.4. Nausea
9.5. Emesis
10. Emesis
10.1. Inducing Emesis: Syrup of Ipecac
10.1.1. Syrup of Ipecac
10.1.1.1. Stimulates serotonin release from EC cells :arrow_right: activates afferent vagus
10.1.2. Indications / Acceptable Use
10.1.2.1. No alternative therapy to decrease GI absorption
10.1.2.2. Can be administered within 30-90 minutes of ingestion
10.2. Vestibular Anti-Emetics
10.2.1. Histamine - H1
10.2.1.1. Diphenhydramine
10.2.1.1.1. Motion-induced nausea mediated by vestibular apparatus
10.2.2. Muscarinic - M1
10.2.2.1. Scopolamine
10.2.2.1.1. Surgeries affecting Vestibular systeem
10.2.2.1.2. Vestibular sensitivty with opioid administration
10.2.2.1.3. Movement after surgery
10.3. PONV Antiemetics
10.3.1. Neuroleptics / Typical Antipschotics
10.3.1.1. Phenothiazines
10.3.1.2. Metoclopramide
10.3.1.2.1. Given with IV dexamethasone for PONV
10.3.1.2.2. Prokinetic Properties :arrow_right: esophageal clearance and gastric emptying
10.3.1.3. Droperidol
10.3.1.3.1. FDA BLACK BOX WARNING
10.3.2. Serotonin 5HT3-R antagonists
10.3.2.1. Contraindications: 1. Congenital Long QT Syndrome 2. SSRI/SNRI - risk of Serotonin Syndrome
10.3.2.2. Dolasetron
10.3.2.3. Ondansetron
10.3.3. Corticosteroids
10.3.3.1. Dexamethasone
10.3.4. Aprepitant
10.3.4.1. 24 Hour Duration
10.3.4.2. Combines with 5HT3 antagonist and dexamethasone if necessary
10.3.5. Dronabinol
10.3.5.1. Medical Marijuana, for refractory chemo NV
10.4. Emesis Mechanisms
10.4.1. Emesis: Key Neurotransmitter Systems
10.4.1.1. Serotonin
10.4.1.2. Neurokinin
10.4.1.3. Histamine - H1
10.4.1.3.1. Diphenhydramine
10.4.1.4. Dopamine - D2
10.4.1.5. Muscarinic - M1
10.4.1.5.1. Scopolamine
10.4.1.6. Opioid - Mu
10.4.1.7. GABA
10.4.1.8. Cannabinoid Receptors
10.4.2. Antiemetics Graphic
10.4.2.1. Antiemetic Therapeutic Sites
10.4.3. Vomiting Center
10.4.3.1. Vomiting Center
