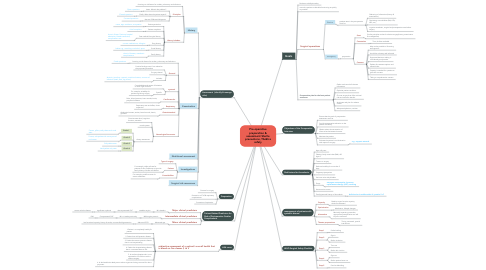
1. Goals
1.1. Reduce morbidly/mortality
1.2. return the patient to desirable functioning as quickly as possible.
1.3. Surgical operations
1.3.1. Elective
1.3.1.1. patients seen in the preoperative clinic for:
1.3.1.1.1. Gathering of information (history & examination).
1.3.1.1.2. Optimizing comorbidities (DM, HTN, IHD, etc.),
1.3.1.1.3. organize anesthetic, surgical and postoperative care before surgery
1.3.2. emergency
1.3.2.1. preparation
1.3.2.1.1. Start
1.3.2.1.2. Constraints
1.3.2.1.3. Consent
1.4. Preoperative plan for the best patient outcomes
1.4.1. Gather and record all relevant information.
1.4.2. Optimize patient condition.
1.4.3. Choose surgery that offers minimal risk and maximum benefit.
1.4.4. Anticipate and plan for adverse events.
1.4.5. Adequate hydration, nutrition
2. Objectives of the Preoperative Interview
2.1. Ensure that the goals of preoperative assessment are met.
2.2. Provide preoperative education to the patient and family.
2.3. Obtain written documentation of informed and witnessed consent.
2.4. Motivate the patient
2.5. Evaluate the patient’s social situation with respect to surgery
2.5.1. e.g., support network
3. Risk factors for thrombosis.
3.1. Age >60 years
3.2. Obesity: body mass index (BMI) >30 kg/m2
3.3. Trauma or surgery
3.4. Reduced mobility for more than 3 days
3.5. Pregnancy/puerperium
3.6. Varicose veins with phlebitis
3.7. Drugs
3.7.1. estrogen contraceptive, hormone replacement therapy (HRT), smoking
3.8. Known active cancer
3.9. Family/personal history of thrombosis
3.9.1. deficiencies in antithrombin III, protein S+C
4. management of patients with systemic disease
4.1. Capacity
4.1.1. Baseline organ function capacity should be assessed
4.2. Optimization
4.2.1. Medication, lifestyle changes
4.3. Alternative
4.3.1. Minimally impacting procedure, appropriate postoperative care will improve outcomes
4.4. Theatre preparations
4.4.1. Timing, teamwork, special instruments
5. WHO Surgical Safety Checklist
5.1. Step 1
5.1.1. Prelist briefing
5.2. Step 2
5.2.1. Sign in
5.2.2. Before induction
5.3. Step 3
5.3.1. Time out
5.3.2. Before skin incision
5.4. Step 4
5.4.1. Sign out
5.4.2. Before patient leave out
5.5. Step 5
5.5.1. Post list debriefing
6. ASA score
6.1. subjective assessment of a patient’s overall health that is based on five classes (I to V
6.1.1. 1-Patient is a completely healthy fit patient
6.1.2. 2. Patient has mild systemic disease.
6.1.3. 3. Patient has severe systemic disease that is not incapacitating.
6.1.4. 4. Patient has incapacitating disease that is a constant threat to life.
6.1.5. 5. A moribund patient who is not expected to live 24 hour with or without surgery.
6.1.6. 6. A declared brain-dead person whose organs are being removed for donor purposes.
7. Assessment (identify & manage risks)
7.1. History
7.1.1. focusing on risk factors for cardiac, pulmonary and infectious
7.1.2. Principles
7.1.2.1. Listen. What is the problem?
7.1.2.1.1. Open questions
7.1.2.2. Clarify. What does the patient expect?
7.1.2.2.1. Closed questions
7.1.2.3. Narrow. Differential diagnosis
7.1.2.3.1. Focused questions
7.1.3. History includes:
7.1.3.1. Patient particulars
7.1.3.1.1. name, age, residence, occupation
7.1.3.2. Patient complains
7.1.3.2.1. chief complains
7.1.3.3. Past medical & surgical history
7.1.3.3.1. chronic illness. Previous hospital admission, blood transfusion, complications etc
7.1.3.4. Drug history
7.1.3.4.1. current medications, allergies
7.1.3.5. Social history
7.1.3.5.1. habits e.g., smocking or alcohol, sport
7.1.3.6. Family history
7.1.3.6.1. chronic illnesses, anesthetic complications
7.2. Examination
7.2.1. focusing on risk factors for cardiac, pulmonary and infectious
7.2.1.1. Fixed questions
7.2.2. General
7.2.2.1. Positive findings even if not related to the proposed procedure
7.2.2.2. Surgery related
7.2.2.3. Includes;
7.2.2.3.1. Anemia, jaundice, cyanosis, nutritional status, sources of infection (teeth, feet, leg ulcers)
7.2.3. systemic
7.2.3.1. Comorbidities and extent of limitation of each organ function.
7.2.3.2. Specific
7.2.3.2.1. For example, suitability for positioning during surgery
7.2.4. Cardiovascular
7.2.4.1. Pulse, blood pressure, heart sounds, bruits, peripheral oedema
7.2.5. Respiratory
7.2.5.1. Respiratory rate and effort, chest expansion
7.2.6. Gastrointestinal
7.2.6.1. Abdominal masses, ascites, bowel sounds, hernia, genitalia
7.2.7. Neurological locomotor
7.2.7.1. Consciousness level, cognitive function, sensation
7.2.7.2. muscle power
7.2.7.3. Airway assessment
7.2.7.3.1. Grade 1
7.2.7.3.2. Grade 2
7.2.7.3.3. Grade 3
7.2.7.3.4. Grade 4
7.3. Nutritional assessment
7.4. Investigations
7.4.1. Type of surgery
7.4.2. Patient
7.4.2.1. For example, sickle cell test for patients of Afro-Caribbean origin with family history of sickle cell disease
7.4.3. Comorbidities
7.4.3.1. For example, peak flow rates for severe asthmatics
7.5. Surgical risk assessmen
8. Preparation
8.1. Consent for surgery
8.2. Prevention of CVS & respiratory complications.
8.3. Prevention of aspiration.
9. Patient-Related Predictors for Risk of Perioperative Cardiac Complications
9.1. Major clinical predictors
9.1.1. MI >6weeks
9.1.1.1. unstable angina
9.1.1.1.1. decompensated CHF
9.2. Intermediate clinical predictors
9.2.1. Mild angina pectoris
9.2.1.1. MI > 6 weeks previously
9.2.1.1.1. Compensated CHF
9.3. Minor clinical predictors
9.3.1. Advanced age
9.3.1.1. Abnormal ECG
9.3.1.1.1. low functional capacity, history of stroke, uncontrolled hypertension
