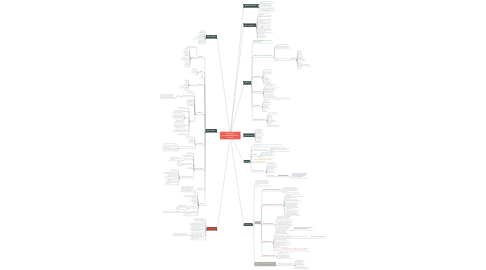
1. History
1.1. Reason for attendance/ main chief complaint (C/C)
1.2. History of the presenting complaint
1.2.1. Listen to the patient - what are their concerns
1.2.2. What do they expect? Is that realistic
1.2.3. If they are in pain, obtain a "pain picture":
1.2.3.1. SOCRATES
1.2.3.1.1. Site
1.2.3.1.2. Onset
1.2.3.1.3. Character
1.2.3.1.4. Radiation
1.2.3.1.5. Associate factors
1.2.3.1.6. Time
1.2.3.1.7. exacerbating/ relieving factors
1.2.3.1.8. Severity
1.3. Dental history
1.3.1. Regular attender?
1.3.2. Previous treatment
1.3.3. L.A
1.3.4. Anxious
1.3.5. Having denture
1.3.6. Periodontalcare
1.4. Medical history
1.4.1. Eg.HIV, AIDS, allergies to latex, anticoagulant therapi
1.4.2. Ability to accept treatment
1.4.3. Ability to give consent
1.4.4. Any drug interaction
1.4.5. Any limit on treatment
1.4.6. Any constraints on treatment items
1.4.6.1. E.g: RPD,epileptic pts
1.5. Social history
1.5.1. Occupation
1.5.2. Family situation
1.5.3. Smoking
1.5.4. Availability
1.5.5. Cost
1.6. Reason for attendance
1.6.1. Look in the notes first
1.6.2. Recall
1.6.3. First visit
1.6.4. Patient initiated
1.6.5. Referral
1.6.6. Who has referred and why
2. Diagnosis
2.1. art of identifying the problem and using scientifc knowledge to determine the cause of the problem.
2.2. Knowledge of the physiology of pain
2.2.1. and methods of interpreting it with available clinical diagnostic devices is essential to reach a proper diagnosis.
2.3. Purpose
2.3.1. to assess the condition of a tooth and object of the patient’s complaint
2.3.2. identify the cause of the pain or discomfort
2.4. Correct pulpal diagnosis is the key to all predictable treatment.
2.5. Diagnosis should be based on:
2.5.1. presenting symptoms
2.5.2. history of symptoms
2.5.3. diagnostic tests
2.5.4. clinical fndings
2.5.5. Rare based on ;
2.5.5.1. single observations
2.5.5.1.1. it is collective analysis and evaluation of the patient’s description of the condition, clinical observations and the results of examinations.
3. Treatment plan
3.1. patient needs most is performed first--with pain, bleeding, and swelling at the beginning of the treatment plan and elective esthetic procedures at the end.
3.2. Stages:
3.2.1. Emergency management (urgent)
3.2.1.1. Treatment of pain / emergencies
3.2.1.2. begins with a thorough review of the patient’s medical history and current condition.
3.2.2. Stabilization phase or Control phase
3.2.2.1. eliminate active disease such as caries and infammation.
3.2.2.2. remove conditions preventing maintenance.
3.2.2.3. eliminate potential causes of disease.
3.2.2.4. remove etiologic factors & OHI.
3.2.2.5. when the patient presents with multiple pressing problems and extensive active disease or when the prognosis is unclear
3.2.2.6. The goals of this phase are to remove etiologic factors, eliminate the ecologic niches of pathogens, and stabilize the patient’s dental health.
3.2.3. Reevaluation Phase
3.2.3.1. time between the control and defnitive phases that allows for resolution of infammation and time for healing.
3.2.3.2. Home care habits are reinforced, motivation for further treatment is assessed, and initial treatment and pulpal responses are re- evaluated before defnitive care is begun
3.2.3.3. Patients with an overall low risk proile, who only require minor alterations in diet, behaviors, and exposure to remineralization agents,—->
3.2.3.3.1. *may not require a formal control phase/reevaluation phase *
3.2.4. Defnitive Phase
3.2.4.1. goes beyond that needed for stabilization of active disease to include restorative treatment design
3.2.4.2. After the dentist reconsiders initial treatment and determines the need for further care, the patient enters the corrective or defnitive phase
3.2.4.2.1. Ex; restorations and rehabilitation.
3.2.4.3. Enhance aesthetics (eg veneers).
3.2.4.4. Provide optimum function (replacement of missing teeth using PD).
3.2.4.5. Resistance to oral stresses (cast restorations).
3.2.4.6. Include:
3.2.4.6.1. endodontic, periodontic, orthodontic oral surgical, and operative procedures before fxed or removable prosthodontic treatment
3.2.5. Maintenance and recall
3.2.5.1. Monitoring / maintenance
3.2.5.2. includes regular reassessment (synonyms include reevaluation, periodic) examinations
3.3. Alteration In The Original Treatment Plan
3.3.1. Several factors may cause an alteration in the original treatment plan which include:
3.3.1.1. The patient’s desire.
3.3.1.2. The oral hygiene.
3.3.1.3. Financial implications.
3.3.1.4. The dentist-patient relationship.
4. Examination
4.1. General
4.1.1. Start before patient sits
4.1.2. Includes:
4.1.2.1. Mobility
4.1.2.2. Demeanour
4.1.2.3. Energy
4.1.2.4. Appearance
4.1.2.5. Level of awareness
4.1.2.6. Attitude
4.1.2.7. Speech
4.1.2.8. Partner
4.2. Facial
4.2.1. Symmetry
4.2.2. Swelling
4.2.3. L.N
4.3. TMJ
4.4. Soft tissue
4.4.1. Systemic:
4.4.1.1. Lips
4.4.1.2. BM
4.4.1.3. Tongue
4.4.1.4. Floor of the mouth
4.4.1.5. Palate
4.5. Periodontal
4.5.1. Oral hygiene
4.5.2. Basic periodontal examination
4.5.2.1. BPE
4.5.2.1.1. simple and rapid screening tool that is used to indicate the level of further examination needed and provide basic guidance on treatment needed.
4.5.3. Probing depth
4.5.4. Bleeding indices
4.5.5. Plaque scores
4.5.6. Codes:
4.5.6.1. 0
4.5.6.1.1. No disease
4.5.6.2. 1
4.5.6.2.1. Bleeding on probing
4.5.6.3. 2
4.5.6.3.1. Supra/sup gingival calculus
4.5.6.3.2. Overhang restoration margin
4.5.6.3.3. Plaque retention factors
4.5.6.3.4. No pocket > 3mm
4.5.6.4. 3
4.5.6.4.1. Shallow pocket 4-5 mm
4.5.6.4.2. Black band seen partly
4.5.6.5. 4
4.5.6.5.1. Deep pocket 6 mm
4.5.6.5.2. Black band disappeared
4.5.6.6. 5
4.5.6.6.1. Furcation
4.6. Prostheses
4.6.1. Does patient wear ?
4.6.2. How long?
4.6.3. How many ?
4.6.4. Does that current denture adaptable?
4.6.4.1. E.g : tolerance of increase face high
4.6.4.2. Is denture needed? Could we accept short dental arch
4.6.4.3. What sort of denture would be best
4.7. Missing teeth
4.7.1. How many ?
4.7.2. how long are the spans?
4.7.3. Where in the arch ?
4.7.3.1. Interpretation the teeth using numbering system like FDI nomenclature.
4.7.4. How long are the span?
4.7.4.1. Short
4.7.4.2. Long
4.7.5. Lost soon ?
4.7.6. Is there already a denture?
4.7.6.1. More are missing
4.7.6.2. Several Edentulous area (long span)
4.7.6.3. Spans more than one unit
4.7.6.4. Other teeth have poor prognosis
4.7.6.5. Denture I already being worn successfully
4.7.6.6. Denture raise the plaque score in both arches
4.8. Occlusion
4.8.1. An occlusal interference is a contact between teeth occurring in certain excursions of the mandible, that interrupts the free sliding movement or guidance normally expected
4.9. Teeth
4.9.1. Caries
4.9.2. Abrasion, Attrition, Erosion? TSL
4.9.3. Appearance
4.9.4. Missing teeth
4.9.5. Vitality
4.9.6. Apical pathology
4.9.6.1. Resorption of the root
4.9.6.2. Previous failure of root canal treatment
4.9.7. Simple restoration
4.9.7.1. Crown
4.9.7.1.1. Bridgework
4.9.8. Plan denture before restoring and crowing
5. Special tests
5.1. Radiographs
5.2. Vitality Tests
5.3. Transillumination
5.4. Photographs
5.5. Study Models
5.6. Blood Tests
6. Conclusion
6.1. Have a systematic approach
6.2. Don't rush into decisions
6.3. Remember pain relief, prevention and periodontal care are the keystones
6.4. You can stage the treatment plan to assess patient compliance
6.5. Always communicate well and inform the patient, gaining consent
6.6. prognosis for each tooth and for the patient's overall dental health.
6.6.1. To establish a prognosis, the practitioner must be able to forecast possible results.
