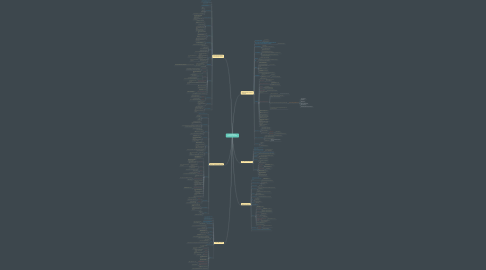
1. Gow Gates nerve Block Technique(open mouth)
1.1. provides anaesthesia to the entire 3rd division of the Mandibular nerve
1.2. has lower incidence of positive aspiration ( 2 % )
1.3. experience of the administrator is very important for this technique
1.4. Nerves Anesthetized
1.4.1. Mental
1.4.2. Incisive
1.4.3. Lingual
1.4.4. Mylohyoid
1.4.5. Auriculotemporal & Buccal ( 75 % of patients )
1.5. Unique Point to Remember
1.5.1. when the mouth is wide open that you have the Condyle very close to the Main nerve trunk of the Mandibular division
1.5.2. after the injection patient has to keep the mouth open
1.6. Areas Anesthetized
1.6.1. Mandibular teeth to the midline
1.6.2. Buccal muco periosteum & mucous membrane
1.6.3. Anterior 2/3rd of tongue
1.6.4. Lingual soft tissues & periosteum
1.6.5. Body of mandible & Inferior portion of Ramus
1.6.6. Skin over the Zygoma, posterior region of cheek & temporal region
1.7. Indications
1.7.1. Multiple procedures on mandibular teeth
1.7.2. Need of soft tissue anaesthesia from 3rd molar to the midline
1.7.3. When lingual soft tissue anaesthesia is required
1.7.4. When Inferior alveolar nerve block has failed
1.8. Contraindications
1.8.1. Infection or acute inflammation in the area of injection
1.8.2. Patients who either bite their lip or has potential for self injury
1.8.3. Patients who are unable to open the mouth wide
1.9. ADV
1.9.1. Requires only 1 injection
1.9.2. High success rate
1.9.3. Minimum risk of +ve aspiration
1.9.4. Few post injection complications
1.9.5. Successful anaesthesia of the Bifid Inf alv nerve & canal
1.10. DisADV
1.10.1. Uncomfortable lingual & lower lip anaesthesia
1.10.2. Longer time of onset of anaesthesia ( Longer than 5 mins )
1.10.2.1. Due to Larger diameter/distance of nerve
1.10.3. Can be frustrating to some people as it has learning curve
1.10.4. Still will need supra-periosteal infiltration for anterior teeth
1.10.4.1. BCZ of cross innervation from the opposite side
1.10.5. Positive aspiration: 2%
1.11. Important Point
1.11.1. important that the patient keeps mouth open even after the deposition of the L.A solution
1.11.1.1. If the mouth is closed immediately after injection, the nerve will move away from the condyle region & anaesthesia will not be effective
1.12. Technique
1.12.1. 25 gauge long needle
1.12.2. Area of insertion
1.12.2.1. Mucous membrane on mesial side of the mandibular ramus
1.12.2.2. On a line from Inter Tragic notch to the corner of the mouth
1.12.3. Target Area
1.12.3.1. Lateral side of condylar neck, just below insertion of Lateral Pterygoid Muscle
1.12.4. Landmark
1.12.4.1. Extra oral
1.12.4.1.1. Lower border of the tragus
1.12.4.1.2. Corner of the mouth
1.12.4.2. Intra oral
1.12.4.2.1. Mesio palatal cusp of max 2nd molar
1.12.4.2.2. Penetration of soft tissue just distal to the Max 2nd molar
1.12.5. Ask patient to extend the neck & open mouth wide why???
1.12.5.1. brings the nerve very close to the condyle
1.12.6. Insert the needle as per the direction determined by the use of the Intra & Extra oral landmarks
1.12.7. Direct the needle towards the target area
1.12.8. Average depth of penetration is 25 mm
1.12.9. Bone contact of the neck of the condyle is made
1.12.10. Volume of solution injected is 1.8 ml
1.12.10.1. If partial anaesthesia develops then another 1.2 ml can be given
1.12.11. Pt should keep the mouth open for 1 – 2 mins after injection
1.13. Signs & Symptoms
1.13.1. Subjective
1.13.1.1. Tingling or numbness of lower lip
1.13.1.2. Tingling or numbness of the tongue
1.13.2. Objective
1.13.2.1. No pain on dental therapy
1.13.2.2. No pain on sharp prick with a sharp probe
1.14. Safety Features
1.14.1. Needle should contact bone, to prevent over penetration
1.14.2. Very low incidence of Positive aspiration
1.15. Failure of Anaesthesia:
1.15.1. rare with Gow Gates Technique
1.15.2. Too little volume of solution is injected initially. Can repeat another 1.2 ml.
1.15.3. Anatomical difficulties – As no bone is contacted
2. Vazirani – Akinosi Closed mouth
2.1. especially useful in cases of Trismus
2.2. Nerves Anesthetized
2.2.1. Inferior alveolar
2.2.2. Incisive & Mental
2.2.3. Lingual
2.2.4. Mylohyoid
2.3. Areas Anaesthetised
2.3.1. Mandibular teeth upto midline
2.3.2. Body of mandible & inferior portion of ramus
2.3.3. Buccal muco-periosteum & mucous membrane anterior to mandibular 1st molar
2.3.4. Anterior 2/3rd of the tongue & floor of oral cavity on the same side
2.3.5. Lingual soft tissue & periosteum
2.4. Indications
2.4.1. Limited mandibular opening
2.4.2. Multiple procedures on mandibular teeth
2.4.3. Inability to visualize landmarks for Inf Alv Nerve block
2.5. Contraindications
2.5.1. Infection or acute inflammation in area of injection
2.5.2. Patient – who might chew or bite the lip or tongue ( like child or mentally handicapped )
2.5.3. Inability to visualize or gain access to the Lingual aspect of Ramus
2.6. ADV
2.6.1. Relatively Atraumatic & patient need not keep the mouth open
2.6.2. Fewer post operative complications ( eg: Trismus )
2.6.3. Lower +ve aspiration (less than 10 %) than that of Inferior alveolar nerve block
2.6.4. Provides good anaesthesia where Bifid Inferior alveolar & canals are present
2.7. DisADV
2.7.1. Difficult to visualize the path
2.7.2. No bony contact
2.7.2.1. Depth of penetration is somewhat arbitrary
2.7.3. Potentially traumatic if needle is too close to the periosteum
2.8. Techniques
2.8.1. 25 gauge long needle is recommended although 27 gauge maybe preferred by dentists
2.8.2. Area of insertion
2.8.2.1. Soft tissue overlying the medial border of ramus of mandible adjacent to the maxillary tuberosity
2.8.2.2. at the height of the muco-gingival junction adjacent to maxillary 3rd molar
2.8.3. Target Area
2.8.3.1. Soft tissue on medial aspect of mandibular ramus
2.8.3.1.1. in region of Inferior alveolar, lingual & mylohyoid nerve
2.8.3.2. run inferiorly from foramen ovale to the mandibular foramen.
2.8.4. Landmark
2.8.4.1. Mucogingival junction of maxillary 3rd or 2nd molar
2.8.4.2. Maxillary tuberosity
2.8.4.3. Coronoid notch on mandibular ramus
2.8.5. Orientation of Bevel
2.8.5.1. should be away from the bone & towards the midline
2.8.6. Place index finger in the coronoid notch
2.8.7. Reflect the tissues for visualization
2.8.7.1. Mucogingival junction of Maxillary 3rd or 2nd molar
2.8.7.2. Maxillary tuberosity
2.8.8. Ask the patient to occlude the teeth with cheeks relaxed
2.8.9. At a height of mucogingival junction of max: 3rd & 2nd molar region
2.8.10. Orient bevel away from bone to the midline
2.8.11. Insert needle for 25 mm into tissues
2.8.11.1. DO NOT over insert the needle ( greater than 25 mm )
2.8.12. Aspirate – If negative deposit 1.5 – 1.8 ml of solution in approximately 1 minute
2.8.13. Motor nerve paralysis develops quickly than sensory
2.8.14. Time for onset of anaesthesia is 40 – 90 seconds
2.8.15. Dental procedure can start after 5 mins
2.9. Signs & Symptoms
2.9.1. Subjective
2.9.1.1. Tingling or numbness of lower lip
2.9.1.2. Tingling or numbness of the tongue
2.9.2. Objective
2.9.2.1. No pain on dental therapy
2.9.2.2. No pain on sharp prick with a sharp probe
2.10. Failure of Anaesthesia
2.10.1. due to flare of the mandible ramus & the site of injection being away from the nerve
2.10.2. Needle insertion point is too low
2.10.3. Under-insertion or Over-insertion of the needle
2.11. Complications
2.11.1. Haematoma
2.11.2. Trismus
2.11.3. Transient facial nerve paralysis
3. Incisive Nerve Block
3.1. nerve is a terminal branch of the Inferior alveolar nerve
3.2. always anesthetized when Inferior alveolar nerve is anesthetized
3.3. technique is useful when bilateral procedure in the mandibular anterior region is indicated , why???
3.3.1. Reason: Bilateral Inferior alveolar nerve block is NOT done
3.4. Nerves Anesthetised:
3.4.1. mental & Incisive nerve
3.5. Areas Anesthetised
3.5.1. Buccal mucous membrane anterior to the mental foramen
3.5.2. Lower lip & chin
3.5.3. Pulp of Premolars, Canine & incisors
3.6. Indications
3.6.1. pulpal Anaesthesia on mandibular teeth anterior to foramen
3.6.2. When IANB is NOT indicated
3.7. Contraindications
3.7.1. Infection or acute inflammation in the area of injection
3.8. ADV
3.8.1. Provides pulpal & hard tissue anaesthesia without lingual anaesthesia
3.8.2. Alternative technique instead of bilateral IANB
3.8.3. High success rate
3.9. DisADV
3.9.1. Does not provide lingual anaesthesia
3.9.2. Partial anaesthesia in the midline region because of cross innervation from the opposite side
3.10. Positive aspiration: 5.7 %
3.11. Technique
3.11.1. 25 or 27 gauge short needle is recommended
3.11.2. Area of insertion
3.11.2.1. mucobuccal fold at or just Anterior to mental foramen
3.11.3. Target area
3.11.3.1. Mental nerve as it exits the mental foramen & Located between the premolars
3.11.4. Landmarks
3.11.4.1. Mandibular premolars & mucobuccal fold
3.11.5. Bevel orientation
3.11.5.1. Towards the bone
3.11.6. Patient position is supine or semi-supine with mouth partially closed
3.11.7. Locate mental foramen and place fingers to retract the cheek
3.11.8. Penetrate the mucosa at right angles & advance the needle
3.11.8.1. Depth of penetration is 5 – 6 mm
3.11.9. Aspirate & On negative aspiration deposit 0.6 ml of solution over 20 seconds
3.11.9.1. apply finger pressure
3.11.10. Apply pressure at injection site for 2 minutes
3.11.11. Withdraw the needle & make safe , Wait 2 – 3 mins for anaesthesia
4. Mental Nerve Block
4.1. terminal branch of the Inferior alveolar nerve after it exits the mental foramen
4.1.1. foramen near the apices of the mandibular premolars
4.2. provides sensory innervation to:
4.2.1. Buccal soft tissues lying anterior to the Foramen
4.2.2. Soft tissues of lower lip
4.2.3. Chin region
4.3. Nerves anesthetized
4.3.1. Mental nerve
4.4. Areas anesthetized
4.4.1. Buccal mucous membrane anterior to mental foramen upto the midline
4.4.2. Skin of lower lip
4.4.3. Chin
4.5. Indications
4.5.1. When soft tissue anaesthesia is needed in anterior mandible
4.5.2. Soft tissue biopsy
4.5.3. Suturing of soft tissue lacerations
4.6. Contraindications
4.6.1. Infection or Acute inflammation in the area of injection
4.7. ADV
4.7.1. High success rate
4.7.2. Technically easy
4.7.3. Usually entirely Atraumatic
4.8. DisADV
4.8.1. Haematoma
4.9. Positive aspiration: 5.7 %
4.10. Technique
4.10.1. 25 or 27 gauge short needle is recommended
4.10.2. Area of insertion
4.10.2.1. mucobuccal fold at or just Anterior to mental foramen
4.10.3. Target area
4.10.3.1. Mental nerve as it exits the mental foramen
4.10.3.2. Mental nerve as it exits the mental foramen
4.10.4. Landmark
4.10.4.1. Mandibular premolars
4.10.4.2. mucobuccal fold
4.10.5. Bevel orientation
4.10.5.1. Towards the bone
4.10.6. Penetrate the mucosa at right angles & advance the needle
4.10.6.1. Depth of penetration is 5 – 6 mm
4.10.7. Aspirate
4.10.7.1. On negative aspiration deposit 0.6 ml of solution over 20 seconds
4.10.8. Withdraw the needle & make safe
4.10.9. Wait 2 – 3 mins for anaesthesia
4.11. Signs & Symptom
4.11.1. Subjective
4.11.1.1. Tingling and numbness of the lower lip
4.11.2. Objective
4.11.2.1. No pain during treatment
4.12. *Do not hit the periosteum with the needle as it can cause pain & discomfort*
5. IAN Block(William Halstead Technique)
5.1. most high chance of failure
5.1.1. 31 – 41 % in molar
5.1.2. 46 % in pre-molars
5.2. IANB + Long Buccal Nerve Block injection, the entire side of the Mandible, Cheek, Tongue & Floor of mouth can be Anesthetized , this called?????
5.2.1. William Halstead Technique
5.3. Nerves Anaesthetised
5.3.1. Inferior alveolar
5.3.2. branch of posterior division of Mandibular nerve
5.3.3. Incisive, mental & Lingual nerve
5.4. Areas Anaesthetised
5.4.1. Mandibular teeth upto midline
5.4.2. Body of mandible & inferior portion of ramus
5.4.3. Buccal muco-periosteum & mucous membrane anterior to mandibular 1st molar
5.4.4. Anterior 2/3rd of the tongue & floor of oral cavity on the same side
5.4.5. Lingual soft tissue & periosteum
5.5. Indications
5.5.1. procedures on multiple mandibular teeth
5.5.2. Where buccal ( ant: to 1st molar ) & lingual soft tissue anaesthesia is required
5.6. ADV
5.6.1. One injection provides a wide area of anaesthesia
5.7. DisADV
5.7.1. Wide area of anaesthesia – Not necessary in localized procedures
5.7.2. High rate of inadequate anaesthesia
5.7.2.1. ( 31 % - 81 % overall )
5.7.3. Intra oral landmarks are NOT always reliable
5.7.4. Highest rate of Positive aspirations ( 10 – 15 % )
5.7.5. Lingual anaesthesia can be dangerous for some patients
5.7.6. Partial anaesthesia possible in cases of a Bifid Inferior alveolar canal
5.8. Contraindications
5.8.1. Infection or acute inflammation in area of injection
5.8.1.1. BCZ of high PH
5.8.2. Patient – who might chew or bite the lip or tongue
5.8.2.1. like child or mentally handicapped
5.9. Technique
5.9.1. 25 gauge long needle is used
5.9.2. Area of insertion
5.9.2.1. Mucous membrane on the medial side of mandibular ramus
5.9.3. Injection is at the intersection of 2 lines
5.9.3.1. One Horizontal ( representing the height of injection )
5.9.3.2. One vertical ( Antero posterior plane of injection )
5.9.4. Target area
5.9.4.1. sulcus mandibularis
5.9.5. Landmarks
5.9.5.1. Coronoid notch, Pterygomandibular raphe & occlusal plane of lower teeth
5.9.6. Orientation of Bevel
5.9.6.1. Not very important but approx.: 90 degrees
5.9.7. Patient is in either supine or semi supine position
5.9.8. Locate the needle penetration site:
5.9.8.1. Determine the height of injection
5.9.8.1.1. Place finger in the Coronoid notch
5.9.8.2. Imaginary line is drawn at the mid point of the finger nail
5.9.8.3. Usually at 6 – 10 mm above occlusal plane
5.9.8.4. The point also is around the mid portion of the Pterygomandibular raphe
5.9.8.4.1. Contents of Pterygomandibular space
5.9.8.5. point of penetration is just lateral to the Pterygomandibular raphe in the Pterygotemporal depression
5.9.9. approach for the injection is from the opposite side premolar region
5.9.10. average depth of penetration is 20 – 25 mm
5.9.11. If the bone is contacted too soon then it is NOT the correct position
5.9.12. When the bone is contacted withdraw 1 mm to prevent Sub-periosteal injection
5.9.13. Aspirate in 2 planes – If negative slowly deposit upto 1.5 ml of solution over 60 sec
5.9.14. Withdraw needle halfway – Aspirate again and deposit 0.1 ml of solution for Lingual N
5.9.15. Wait for 3 – 5 minutes for the Anaesthesia to work
5.10. Signs & Symptoms
5.10.1. Tingling or numbness of the lower lip
5.10.2. Tingling or numbness of the Tongue
5.10.3. No pain on dental therapy
5.10.4. Clinician has to check for
5.10.4.1. Subjective signs
5.10.4.1.1. What the patient says
5.10.4.2. Objective signs
5.10.4.2.1. with a sharp probe ( What clinician finds out )
5.11. Reasons for failure of Anaesthesia
5.11.1. solution is injected too low or below the level of the Mandibular foramen
5.11.2. solution is deposited too far anteriorly
5.11.3. Rarely – A Bifid Inferior alveolar nerve
5.11.4. anterior region
5.11.4.1. due to the cross innervation from the opposite side
5.12. Complications
5.12.1. Haematoma
5.12.2. Trismus
5.12.3. Transient facial nerve paralysis
6. Long Buccal Nerve Block
6.1. branch of the Anterior division of the mandibular nerve
6.2. NOT always necessary to anesthetize this nerve in all restorative procedures
6.2.1. while performing surgery on the Molars it is VERY ESSENTIAL
6.3. supplies the Buccal mucosa & periodontium in the region of 1st, 2nd & 3rd molars
6.4. Indications
6.4.1. When buccal soft tissue anaesthesia is required for the molar region
6.5. Contraindications
6.5.1. Infection or acute inflammation of the area of injection
6.6. Advantages
6.6.1. High success rate & Technically easy
6.7. Disadvantages
6.7.1. Potential for pain if needle contacts bone
6.7.2. injection becomes Subperiosteal & painful
6.8. Techniques
6.8.1. 25 Gauge long needle is used
6.8.2. Area of insertion
6.8.2.1. mucous membrane distal & buccal to the most distal tooth
6.8.3. Target area
6.8.3.1. Buccal nerve as it passes over the anterior or border of Ramus
6.8.4. Orientation of Bevel
6.8.4.1. Towards the bone
6.8.5. Retract the cheek with the right finger to improve the visibility
6.8.6. Keep the needle parallel to the occlusal plane & penetrate the mucosa
6.8.7. Contact the bone , Aspirate & Inject 0.3 ml of solution over 10 seconds
