1. Discharge
1.1. Discharge Medication (Frandsen & Pennington, 2021)
1.1.1. Empagliflozin: SGLT2 inhibition, reduces reabsorption of glucose and increases urinary excretion of glucose. Teaching: Medication can cause dehydration, recognize signs of low blood sugar (dizziness, lightheadedness, fainting)
1.1.2. Sitagliptin/metformin: Reduces absorption of glucose from the stomach, increases pancreatic insulin release. Teaching: Take with meals, exercise regularly and eat a balanced diet.
1.1.3. Valsartan: ARB for HTN and HF management Teaching: NSAIDs may interact with valsartan, get out of bed slowly and rest feet on the floor before standing up.
1.1.4. Clopidogrel: platelet inhibitor Teaching: avoid falls and avoid contact sports, avoid NSAIDs
1.1.5. Atorvastatin: lowers cholesterol levels Teaching: Take at same time each day, avoid foods high in fat
1.1.6. Advair Discus: Fluticasone/Salmererol. Targets immune response, reduces inflammation in airway, relaxes lung muscles Teaching: Rinse mouth with water after each dose, take twice a day 12 hours apart
1.2. Discharge Teaching
1.2.1. Lifestyle recommendations: Decrease salt intake, incorporate 150 minutes of mild to moderate exercise per week (walking and body weight exercises are free).Avoid large crowds and people who have known or suspected sickness Social Determinants of Health Recommendations: Utilize community resources such as food banks. Apply for medicaid for financial assistance to stay compliant with prescribed medications (Honan, 2019)
1.2.1.1. Call provider if... Your weight increases by 2lbs in a day or 5lbs in a week. You have trouble breathing. You notice swelling in your feet or ankles. You feel your heart beating unusually fast or slow.
1.2.2. Medication Comparison: the new medication is Warfarin. Limit intake of dark leafy greens, grapefruit juice, alcohol. No contact sports, watch for signs of bleeding-> bruising, lightheadedness, weakness (Frandsen & Pennington, 2021).
2. DMT2
3. Heart Failure
4. DVT
5. Bronchitis/Emphysema
6. Care Plan Interventions
6.1. Medications (Frandsen & Pennington, 2021)
6.1.1. Heparin and Warfarin used as prophylaxis and treatment of blood clots especially during sedation and mechanical ventilation
6.1.2. Insulin is used to transport glucose into the cells so it can be used for energy
6.1.3. Furosemide is a potassium-wasting diuretic used to decrease fluid volume, thereby decreasing edema and fluid in the lungs
6.1.4. Pantoprazole is a proton-pump inhibitor used to prevent gastric ulcers during mechanical ventilation
6.1.5. Amiodarone is an antiarrhythmic used to treat atrial fibrillation
6.1.6. Dexemedetomidine, Midazolam, and Hydromorphone are used for sedation during intubation and mechanical ventilation
6.2. Nursing Tasks
6.2.1. Determine and address any cultural and language barriers when accessing care and implementing lifestyle modifications.
6.2.2. Safety: sterile water and occlusive dressing at bedside for chest tube, bed alarm on, continuous cardiac and respiratory monitoring, monitor aPTT before giving heparin,HOB at 30 when administering tube feed
6.2.3. Strict I/O monitoring
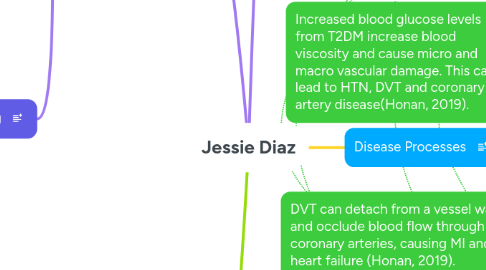
7. DVT can detach from a vessel wall and occlude blood flow through coronary arteries, causing MI and heart failure (Honan, 2019).
8. Emphysema, a subset of COPD, can lead to pulmonary HTN and eventually right sided heart failure (Honan, 2019)
9. Increased blood glucose levels from T2DM increase blood viscosity and cause micro and macro vascular damage. This can lead to HTN, DVT and coronary artery disease(Honan, 2019).
10. Incre
11. M
12. Smoking irritates alveolar and bronchiolar walls, causing hypersecretion of mucus, inflammation, and fibrotic changes which significantly decrease gas exchange (Honan, 2019).
13. Atherosclerosis and HTN decrease perfusion and cause compensatory mechanisms to activate, causing further vasoconstricton and decreased cardiac output and perfusion (Honan, 2019).
14. Non ST Segment Elevation Myocardial Infarction: Occurs due to occlusion of coronary arteries, decreasing perfusion and oxygenation to cardiac cells (Honan, 2019).
15. Hyperlipidema
16. DMT2
17. Pulmonary edema
18. Assessment
18.1. Symptoms
18.1.1. Right leg pain
18.1.2. Increasing SOB
18.1.3. Worsening cough w/thick pink mucus
18.1.4. Crackles in lungs
18.1.5. Upper and lower extremity edema
18.1.6. Vitals: high and irregular HR, high RR, low MAP, low pulse ox
18.2. Labs/Diagnostics
18.2.1. 15% Pneumothorax apex of right lung and RUL infiltrate
18.2.2. Total cholesterol: 230mg/dL and LDL total 196mg/dL
18.2.3. Elevated creatinine (1.4-1.7 mg/dL)
18.2.4. Troponin 2.4ng/mL
18.2.5. NT-proBNP 242 pg/mL
18.2.6. Upon admission, ABG results: PCO2 52 mmHg, pH 7.31, PaO2 64mmHg, HCO3 19mEq/L
18.2.7. Elevated blood glucose (235 mg/dL)
19. Smoking 1 pack a day for 38 years: Damages blood vessel walls and increases plaque build-up (Honan, 2019)
20. Drinking wine socially: Can cause increased cholesterol (Honan,2019).
21. Heart failure
22. Disease Processes
22.1. Heart Failure: the demand of the body exceeds the heart's ability to pump enough blood (Honan, 2019)
22.1.1. Pulmonary edema: Fluid retention due to HF causes pulmonary edema (Honan,2019). It can lead to respiratory distress and possible respiratory failure.
22.1.1.1. Atrial Fibrillation: Abnormal electrical activity of the heart causing extremely fast atrial contractions. Significantly decreases cardiac output(Honan, 2019).
22.2. Atherosclerosis: depositing of plaque on blood vessel walls (Honan, 2019).
22.2.1. Hypertension: increases workload of heart, decreases perfusion (Honan, 2019)
22.2.1.1. Coronary Artery Disease: Accumulation of plaque in coronary arteries leading to decreased perfusion to cardiac cells(Honan, 2019). Can progress to unstable angina, NSTEMI and STEMI, and then heart failure
