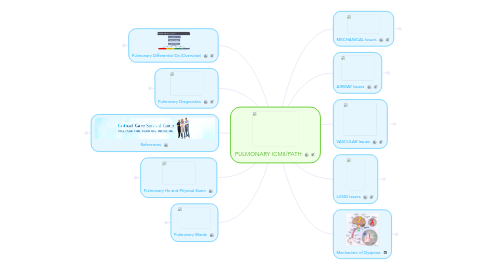
1. Pulmonary Differential Dx (Overview)
1.1. LUNG
1.1.1. Atelectasis
1.1.1.1. Definition: "Collapsed Lung"
1.1.1.2. Causes of Atelectasis
1.1.1.2.1. 1. Pleural Effusion
1.1.1.2.2. 2. Penumothorax
1.1.1.2.3. 3. Mucus Plugging
1.1.1.2.4. 4. Poor Respiratory Efforts
1.1.1.3. Damage: Can cause hypoxia because of mismatch abnormalities; however, it does NOT cause FEVER!
1.1.2. Common symptoms: Cough, Pleuritic Pain, Crackles, Infiltrate on CXR, Decreased DLCO
1.2. VASCULAR
1.2.1. Common symptoms: Leg Edema, Crackles, Decreased DLCO, Elevated D-dimer
1.3. AIRWAY
1.3.1. Common symptoms: Cough, Wheeze, Decreased DLCO
1.4. MECHANICAL
1.4.1. Common symptoms: Pleuritic Pain, Decreased DLCO, Positive "sniff" test
2. Pulmonary Diagnostics
2.1. Aterial Blood Gas (ABG)
2.1.1. ABG= pH, PaCO2, PaO2
2.1.1.1. (measure of dissolved molecules)
2.1.1.1.1. The ABG relationship between pH, PaCO2, and PaO2 are represented by the Henderson-Hasselbach Equation.
2.1.1.2. Allen's Test must be performed to ensure both radial and ulnar circulation to the hand before starting an arterial line (in order to get an ABG). Without both circulation the patient is at increased risk for thrombosis in the hand leading to infarction.
2.1.1.3. 3 components of ABG
2.1.1.3.1. pH (normal = 7.4)
2.1.1.3.2. PaCO2 (normal = 40)
2.1.1.3.3. PaO2 (normal ~ 100)
2.1.2. Clinical Questions
2.1.2.1. 1. What is wrong with the patient that has a pH > 7.4 with a PaCO2 > 40?
2.1.2.1.1. Remember: You never over compensate when it comes to your pH!
2.1.2.1.2. Either there is a primary metabolic alkalosis with respiratory compensation OR there is both a metabolic alkalosis and a respiratory acidosis. How would you sort this out?
2.1.2.2. 2. You are called to a rapid response to find a 34 year old female s/p cervical fusion. She was on a morphine PCA. Her oxygen saturations are decreased (89%) on room air. You are trying to figure out if you should give her narcan (reverse morphine effect) or send her to CT to rule out Pulmonary Embolism. You order an ABG: 7.20/65/60 on room air. What next doctor? Does hypoventilation effect oxygenation?
2.1.2.2.1. A-a gradient = Alveolar Oxygen – Arterial Oxygen
2.1.2.2.2. If our patients A-a gradient is abnormal (elevated) it would suggest that she has a PE or some other gas exchange problem (atelectasis) in addition to hypoventilation (morphine) as the cause of her hypoxia.
2.1.2.2.3. If our patients A-a gradient is abnormal (elevated) it would suggest that she has a PE or some other gas exchange problem (atelectasis) in addition to hypoventilation (morphine) as the cause of her hypoxia.
2.1.2.2.4. A-a gradient = Alveolar Oxygen – Arterial Oxygen
2.2. Pulmonary Function Tests (PFT)
2.3. Swan-Ganz Catherization
3. References
3.1. http://www.youtube.com/user/IUCriticalCare IU Critical Care Video Homepage
3.2. http://www.youtube.com/watch?v=_hjD566XOO0 Emphysema Intro
3.3. http://www.youtube.com/watch?v=ChlSfDBHLvg Emphysema Pathophysiology
3.4. http://www.youtube.com/watch?v=l_xZrdyK1-s Emphysema Treatment
3.5. http://www.youtube.com/watch?v=i-sZzZ4TMnY Pneumothorax Explained!
3.6. http://www.youtube.com/watch?v=38rHuxIhf6I Tension Pneumothorax TREATMENT
3.7. http://www.youtube.com/watch?v=z0dCL4CHGSk Thorocentesis Medical Animation
3.8. http://www.youtube.com/watch?v=v9-9MfJMtyg Acid/Base Disorders
3.9. http://www.youtube.com/user/MEDCRAMvideos/videos Pulmonary Videos are great!
4. Pulmonary Hx and Physical Exam
4.1. Case-Based Approach
4.1.1. Patient Mr. C
4.1.1.1. History
4.1.1.1.1. Mr. C is a 64y/o man who presents with Shortness of Breath (S.O.B.)- Over the last 2 years he has noticed increasing dyspnea on exertion. He is now S.O.B. with minimal exertion. Lying flat exacerbates his symptoms and he sleeps on 3 pillows. He has noticed associated lower extremity edema. On occasion he awakens from sleep acutely short of breath.
4.1.1.1.2. What do we want to know about Mr. C's pulmonary history?
4.1.1.2. Creating a Differential requires us to utilize the Airway, Vascular, Lung, Mechanical thought process.
4.1.1.3. CXR for Mr. C- positive for Pulmonary Edema
4.1.1.4. Mr. C's Diff Dx category: VASCULAR
4.1.2. Patient Mrs. W
4.1.2.1. History
4.1.2.1.1. Mrs. W is an obese 40 y/o female who presents with a cough of 2 months duration. Her cough is non-productive and NOT associated with fever or shortness of breath (S.O.B.). She does not wheeze. She has tried OTC anti-histamines without relief. Mrs. W denies rhinorrhea, pharyngitis, heartburn, and weight loss. She does note that her cough seems to get worse after her water aerobics class.
4.1.2.1.2. What other questions would help narrow down the cause of this patient's cough?
4.1.2.1.3. Need to consider in Social History
4.1.2.1.4. Need to consider in Family History
4.1.2.2. Creating a Differential requires us to utilize the Airway, Vascular, Lung, Mechanical thought process.
4.1.2.3. Mrs. W's Chest CT- showing pulmonary infiltration characteristic of Hypersentitivity pneumonitis. Dx: Mycobacterium avium complex antigen (most likely contracted the microbe from her water aerobics class.)
4.2. Pulmonary Physical Exam
4.2.1. Inspection
4.2.1.1. Nasal flaring, pursed lips (COPD/emphysema), sentence length and cadence, abdominal breathing.
4.2.1.2. Accessory muscles being utilized to breath (Scalene and Sternocleidomastoid (SCM))
4.2.1.3. Kyphoscoliosis, clubbing, edema
4.2.2. Percussion (use your wrist!)
4.2.2.1. Side to side, hyper or hypo resonance.
4.2.3. Auscultation
4.2.3.1. Types of breath sounds
4.2.3.1.1. Vesicular (normal or soft)
4.2.3.1.2. Tracheal (harsh, loud) stridor =inspiratory
4.2.3.1.3. Bronchial (loud, air through a tube)
4.2.3.1.4. Bronchial (loud, air through a tube)
4.2.3.1.5. Wheeze (high pitch, end expiratory)
4.2.3.1.6. Velcro (fibrosis, like a Velcro sneaker)
4.2.3.1.7. Rhonchi (low pitched, mucus plugging)
4.2.3.1.8. Crackels or rales or creeps (expiratory or inspiratory, like rubbing hair in-between fingers opening sounds of alveoli)
4.2.3.2. Egophony ("eeee"-->"aaaa" transition = consolidation in the lung.)
4.2.3.3. Whisper Pectoriloquy ("toy boat"- if hear louder through the patients back then this is indicative of lung consolidation over that lung field).
5. Pulmonary Wards
5.1. Case-Based Approach
5.1.1. Patient Mr. Lebanon
5.1.1.1. History
5.1.1.1.1. CC: Dyspnea for 2 yrs
5.1.1.1.2. HPI: Mr. Lebanon is a 66 year old white male farmer who has noticed increased work of breathing while bailing hay and walking around the farm. His shortness of breath has gradually been worsening. Mild intermittent non-productive cough. He smokes ½ ppd. He does not notice a seasonal or geographic correlation with his symptoms. His symptoms improve only with rest. He was given an albuterol inhaler by his PCP which does not seem to help so he does not use it.
5.1.1.1.3. Social History
5.1.1.1.4. HPI (cont...) and Positive Review of Systems (ROS)
5.1.1.1.5. PMHx / Medications
5.1.1.1.6. Family History
5.1.1.2. ROS
5.1.1.2.1. Gen – 10 lb weight loss over 2 months, fatigued Cardiac – neg Pulmonary – per HPI, also denies hemoptysis Gastro – neg Skin – neg MSK – low back pain with bending/lifting Psych – denies depression, anxiety Neuro – neg GU – neg HEENT – neg, denies rhinitis
5.1.1.3. Physical Exam
5.1.1.3.1. V: HR 88, RR 18, 118/76, Sat 88% RA Gen: non-anxious, smells of cigarettes Pul: bilateral coarse rales Car: RRR w/o obv m/r/g Neu: no focal deficits MSK: ---> Skin: no rashes Psy: normal affect HEENT: oropharynx clear, no rhinitis
5.1.1.4. Labs/Imaging
5.1.1.4.1. Na 136 K 4.9 Cl 98 CO2 28 Glu 104 BUN 15 Cr 0.7 HgB 14.6 WBC 10 Plt 334
5.1.1.4.2. What Next? What Dx are we suspicious of? What data can help narrow in on our diagnosis?
5.1.1.4.3. Based on an abnormal CXR we want to get a chest CT!
5.1.1.4.4. Too many interstitial markings! This a reticular pattern- because the fine markings are all connected. Both lungs are involved and the lower lobes are involved the most bilaterally.
5.1.1.5. Pop-Quiz!!!
5.1.1.5.1. Question 1
5.1.1.5.2. Question 2
5.1.1.5.3. Question 3
5.1.1.5.4. Question 4
5.1.1.5.5. Question 5 "Why is it fun to be a Pulmonologist?!"
5.1.2. Patient Ms. R
5.1.2.1. History
5.1.2.1.1. CC: Dyspnea w/ Exercise
5.1.2.1.2. 30 y/o female marathon runner. She states that when she is running she starts out well, but then starts to feel fatigued and short of breath not long after.
5.1.2.1.3. More Hx
5.1.2.2. Based on the Patient's History....
5.1.2.2.1. Answer: B. Exercise Induced Asthma
5.1.2.2.2. What must we make sure that we consider when developing a diffential diagnosis for this patient?
5.1.2.3. Treatment for Ms. R
5.1.2.3.1. Answer: A. Albuterol MDI & Montelukast- this is well used. Also we can give B. Albuterol MDI & fluticasone/salmeterol inhaler! Note: NEVER GIVE A LONG ACTING BETA AGONIST WITHOUT A GLUCOCORTICOID!
5.1.2.4. Rest of the Story!!!!
5.1.2.4.1. We provided our patient w/ 2 prescriptions and educated her with regards to her asthma. She returned several months later after having won gold at eh 2012 Summer Olympic Games.
5.1.3. Patient Mr. X
5.1.3.1. History
5.1.3.1.1. CC: "Shortness of breath when walking"
5.1.3.1.2. 65y/o male secret government agent who specializes in hiding the 'truth' from the American people. Mr. X is a 70 pack-year smoker who currently still smokes 2ppd. He recently returned from a trip to Roswell, NM. He admits to 10lb unintentional weight loss over the last few months, a dry cough, and increased fatigue.
5.1.3.1.3. More History
5.1.3.2. Physical Exam: shows nicotine stains on fingers and abnormal O2 saturation (low)
5.1.3.2.1. Lab value and CXR- the lung fields are hypodense
5.1.3.2.2. Lung Function Tests
5.1.3.3. Based on the Patients History, PE, and Lab/tests...
5.1.3.3.1. Answer: B. Emphysema w/ a compound of asthma (a little)
5.1.3.4. Follow Up CXR- showing an abnormal hilary mass w/ some tracheal deviation.
5.1.3.4.1. Chest CT- shows increased lymphadenopathy and a cavity lesion.
5.1.3.5. Treatment of Mr. X
5.1.3.5.1. Quit smoking. We must discuss the next steps for cancer evaluation.
5.2. A closure look at Obstructive Lung Disease
5.2.1. Ms. R has a form of Obstructive Disease. What are some other causes of Airway Obstruction? (Air Can't Get Out)
5.2.1.1. Emyphysema
5.2.1.1.1. Neurtophil elastase---> destroy alveoli and elastic recoiling leading to hyperinflation (irreversible)
5.2.1.2. Chronic bronchitis
5.2.1.2.1. Musuc hypersecretion (irritants)---> physical obstruction & chronic productive cough (3mons > 2 yrs)
5.2.1.3. Asthma
5.2.1.3.1. Airway inflammation + bronchial hyperresponsiveness---> constriction leading to air-trapping (reversible).
5.2.2. Overlap --> How to distinguish features of COPD
5.2.2.1. Distinguishing features
5.2.2.1.1. History
5.2.2.1.2. Physical Exam
5.2.2.1.3. Diagnostic test
6. MECHANICAL Issues
6.1. Pleural Disease
6.1.1. Pneumothorax
6.1.1.1. Spontaneous Pneumothorax
6.1.1.1.1. Primary
6.1.1.1.2. Secondary
6.1.1.2. Tension pneumothorax
6.1.2. Mesothelioma
7. AIRWAY Issues
7.1. Nasopharynx
7.2. Larynx
7.3. Chronic Obstructive Pulmonary Disease (COPD)
7.4. Respiratory Distress Syndromes
8. VASCULAR Issues
8.1. Pulmonary Hypertension (Pulm HTN)
8.1.1. Primary Pulmonary HTN
8.1.2. Secondary Pulmonary HTN
8.2. Pulmonary Embolism
8.3. Left to Right Shunts
9. LUNG Issues
9.1. Pulmonary Infectious Diseases
9.2. Restrictive Diseases
9.3. Lung Cancer
10. Mechanism of Dyspnea
10.1. Peripheral Receptors ("Non-Brain")
10.1.1. 1. Chest wall mecahnoreceptors
10.1.1.1. These are muscle spindles and tendons. They sense tension and contraction of the sternocleidomastoid muscles, scalene muscles, diaphragm, and intercostals.
10.1.2. 2. Chemoreceptors
10.1.2.1. These receptors are located in the aorta and carotide bodies. They provide the sensation of dyspnea from high CO2, low pH, or low O2 levels in the blood.
10.1.3. 3. Lung receptors
10.1.3.1. These receptors communicate with the bronchopulmonary vagal c-fibers that do NOT transmit pain! Cough and stretch reflexes are mediated through these receptors.
10.2. Central Mechanisms ("Brain")
10.2.1. All aspects of central processing of peripheral receptor information is not clear; however, fMRI data shows dyspnea in R-insular region of the amygdala. Additionally, pH and pCO2 of the brain in the interstitial fluid of the brain has an affect of central mechanisms of dyspnea.
10.2.1.1. Odine's Curse
10.2.1.1.1. Congenital central hypoventilation syndrome
10.2.1.1.2. Caused by Trauma and Brainstem surgery ( done in 1962)
10.2.1.1.3. factoid: based on german folklore long before the official discovery of this diagnosis.
10.2.1.1.4. Presents: Loss of autonomic control of breathing results in the need to consciously initate every breath. (If the patient fell asleep they would die- ergo the curse.
