1. B. Patient Outcomes
1.1. Type of Harm
1.1.1. Clinical or Environmental Injury
1.1.2. Traumatic Injury
1.1.3. Infections and Infestations
1.1.4. Pathophysiology
1.1.4.1. Blood and Lymphatic Disorders
1.1.4.2. Cardiac Disorders
1.1.4.3. Ear and Labyrinth Disorders
1.1.4.4. Endocrine Disorders
1.1.4.5. Eye Disorders
1.1.4.6. Gastrointestinal Disorders
1.1.4.7. Hepatobiliary Disorders
1.1.4.8. Immune System Disorders
1.1.4.9. Metabolism and Nutrition Disorders
1.1.4.10. Musculoskeletal and Connective Tissue Disorders
1.1.4.11. Nervous System Disorders
1.1.4.12. Pregnancy, Puerperium, and Perinatal / Congenital Conditions
1.1.4.13. Psychiatric Disorders
1.1.4.14. Renal and Urinary Disorders
1.1.4.15. Reproductive Systems and Breast Disorders
1.1.4.16. Respiratory, Thoracic, and Mediastinal Disorders
1.1.4.17. Skin and Subcutaneous Tissue Disorders
1.1.4.18. Vascular Disorders
1.1.5. Undefined or Unknown Location
1.2. Cause or Mechanism of Harm
1.2.1. Procedural Complications
1.2.2. Environmental Injury
1.2.3. Traumatic Injury
1.2.4. Infection or Infestation
1.2.5. Poisoning and Ingestion
1.2.6. Deterioration of Underlying Illness
1.3. Extent of Harm
1.3.1. None
1.3.2. Mild
1.3.3. Moderate
1.3.4. Severe
1.3.5. Death
2. A. Incident Type
2.1. Administration
2.1.1. Patient Identification
2.1.1.1. Not Performed
2.1.1.2. Incomplete
2.1.1.3. Incorrect
2.1.2. Consent
2.1.2.1. Not Performed
2.1.2.2. Incomplete
2.1.2.3. Incorrect
2.1.3. Coding / Coordination / Screening in Ornge Communication Centre
2.1.3.1. Launch Delay
2.1.3.2. Service Delay
2.1.3.3. Inadequate Equipment Communication
2.1.3.4. Refusal
2.1.3.5. Alternate Dispatch
2.1.3.6. No Consult with TMP
2.1.3.7. No Follow-up with Sending / Receiving
2.1.3.8. Improper Waste Disposal (Sharps, Biomedical, Hazardous Materials)
2.1.4. Resources / Organizational Management
2.1.4.1. Alignment of Workload Management - hours of work, # of calls, acuity, work scheduling
2.1.4.2. Service Availability / Adequacy (Ornge)
2.1.4.3. Human Resource / Staff Availability / Adequacy / Levels
2.1.4.4. Organization of Teams / People
2.1.4.5. Protocols / Policy / Procedure / Guideline Availability / Adequacy
2.1.4.6. External Resources
2.1.5. Task Allocation
2.1.5.1. Not Performed
2.1.5.2. Incomplete
2.1.5.3. Incorrect
2.1.6. Documentation
2.1.6.1. Orders / Requests
2.1.6.1.1. Missing or Unavailable Document
2.1.6.1.2. Delay in Accessing Document
2.1.6.1.3. Wrong Patient
2.1.6.1.4. Unclear / Ambiguous / Illegible / Incomplete Information
2.1.6.1.5. Wrong Document
2.1.6.1.6. Delay in Completing Document
2.1.6.2. Medical Records / AACR / ePCR
2.1.6.2.1. Missing or Unavailable Document
2.1.6.2.2. Delay in Accessing Document
2.1.6.2.3. Wrong Patient
2.1.6.2.4. Unclear / Ambiguous / Illegible / Incomplete Information
2.1.6.2.5. Wrong Document
2.1.6.2.6. Delay in Completing Document
2.1.6.3. Checklists
2.1.6.3.1. Missing or Unavailable Document
2.1.6.3.2. Delay in Accessing Document
2.1.6.3.3. Wrong Patient
2.1.6.3.4. Unclear / Ambiguous / Illegible / Incomplete Information
2.1.6.3.5. Wrong Document
2.1.6.3.6. Delay in Completing Document
2.1.6.4. Forms / Certificates
2.1.6.4.1. Missing or Unavailable Document
2.1.6.4.2. Delay in Accessing Document
2.1.6.4.3. Wrong Patient
2.1.6.4.4. Unclear / Ambiguous / Illegible / Incomplete Information
2.1.6.4.5. Wrong Document
2.1.6.4.6. Delay in Completing Document
2.1.6.5. Instructions / Information / Policies / Procedures / Guidelines
2.1.6.5.1. Missing or Unavailable Document
2.1.6.5.2. Delay in Accessing Document
2.1.6.5.3. Wrong Patient
2.1.6.5.4. Unclear / Ambiguous / Illegible / Incomplete Information
2.1.6.5.5. Wrong Document
2.1.6.5.6. Delay in Completing Document
2.1.6.6. Labels / Stickers / Identification Bands / Cards
2.1.6.6.1. Missing or Unavailable Document
2.1.6.6.2. Delay in Accessing Document
2.1.6.6.3. Wrong Patient
2.1.6.6.4. Unclear / Ambiguous / Illegible / Incomplete Information
2.1.6.6.5. Wrong Document
2.1.6.6.6. Delay in Completing Document
2.1.6.7. Letters / E-mails / Records of Communication
2.1.6.7.1. Missing or Unavailable Document
2.1.6.7.2. Delay in Accessing Document
2.1.6.7.3. Wrong Patient
2.1.6.7.4. Unclear / Ambiguous / Illegible / Incomplete Information
2.1.6.7.5. Wrong Document
2.1.6.7.6. Delay in Completing Document
2.1.6.8. Reports / Results / Images
2.1.6.8.1. Missing or Unavailable Document
2.1.6.8.2. Delay in Accessing Document
2.1.6.8.3. Wrong Patient
2.1.6.8.4. Unclear / Ambiguous / Illegible / Incomplete Information
2.1.6.8.5. Wrong Document
2.1.6.8.6. Delay in Completing Document
2.1.6.9. OCC Software / Resources*
2.1.6.9.1. Missing or Unavailable Document
2.1.6.9.2. Delay in Accessing Document
2.1.6.9.3. Wrong Patient
2.1.6.9.4. Unclear / Ambiguous / Illegible / Incomplete Information
2.1.6.9.5. Wrong Document
2.1.6.9.6. Delay in Completing Document
2.1.7. Appointment / Referral / Consultation
2.1.7.1. Not Performed
2.1.7.2. Incomplete
2.1.7.3. Incorrect
2.2. Transfer / Handover
2.2.1. Handover / Transfer of Care to Ornge Personnel
2.2.1.1. Not Performed
2.2.1.2. Incomplete
2.2.1.3. Incorrect
2.2.2. Handover / Transfer of Care from Ornge Personnel
2.2.2.1. Not Performed
2.2.2.2. Incomplete
2.2.2.3. Incorrect
2.2.3. Handover to OCC Personnel
2.2.3.1. Not Performed
2.2.3.2. Incomplete
2.2.3.3. Incorrect
2.2.3.4. Coding/Coordination/Screening in OCC
2.2.3.4.1. Launch Delay
2.2.3.4.2. Service Delay
2.2.3.4.3. Inadequate Equipment Communication
2.2.3.4.4. Refusal
2.2.3.4.5. Alternate Dispatch
2.2.3.4.6. No Consult with TMP
2.2.3.4.7. No Follow-up with Sending / Receiving
2.2.3.4.8. Improper Waste Disposal (Sharps, Biomedical, Hazardous Materials)
2.3. While in Ornge Care
2.3.1. Accident & Accident Effect
2.3.1.1. Threat to Airway
2.3.1.2. Threat to Breathing
2.3.1.3. Threat to Circulation
2.3.1.4. Blunt Force
2.3.1.5. Piercing / Penetrating Force
2.3.1.6. Excessive Heat / Cold
2.3.1.7. Asset Damage
2.3.1.7.1. Facility Damage
2.3.1.7.2. Facilities Inventory Type
2.3.1.7.3. Vehicle Damage
2.3.1.7.4. Vehicle Inventory Type
2.3.1.8. Other
2.3.1.8.1. Exposure to Electricity / Radiation
2.3.1.8.2. Exposure to Sound / Vibration
2.3.1.8.3. Exposure to Air Pressure
2.3.1.8.4. Exposure to Chemical or Other Substance
2.3.1.8.5. Exposure to Low Gravity
2.3.1.8.6. Exposure to (Effect of) Weather, Natural Disaster, or Other Force of Nature
2.3.1.8.7. Struck by Explosive Blast
2.3.1.8.8. Contact with Machinery
2.3.2. Inappropriate Behaviour
2.3.2.1. Patient
2.3.2.1.1. Uncooperative
2.3.2.1.2. Aggressive
2.3.2.1.3. Assault
2.3.2.2. Family
2.3.2.2.1. Uncooperative
2.3.2.2.2. Aggressive
2.3.2.2.3. Assault
2.3.2.3. Ornge Personnel
2.3.2.3.1. Uncooperative
2.3.2.3.2. Aggressive
2.3.2.3.3. Assault
2.3.2.4. Other Personnel
2.3.2.4.1. Uncooperative
2.3.2.4.2. Aggressive
2.3.2.4.3. Assault
2.3.3. Error in Process / Procedure
2.3.3.1. Procedural Error
2.3.3.1.1. Screening / Prevention / Routine Check
2.3.3.1.2. Procedure / Treatment / Intervention
2.3.3.1.3. General Care / Management
2.3.3.1.4. Detention / Restraint
2.3.3.1.5. Diagnosis / Assessment
2.3.3.1.6. Tests / Investigations
2.3.3.1.7. Response to Emergency / Immediate Threat to Life
2.3.3.2. Equipment / Consumable Error
2.3.3.2.1. Infection Control Barrier
2.3.3.2.2. Medication / IV Fluids
2.3.3.2.3. Medical Device / Equipment
2.3.3.2.4. Oxygen / Gas / Vapour
2.3.3.2.5. Blood / Blood Products
2.3.3.2.6. Specimens / Results
2.3.4. Organ Donation
2.3.4.1. Service Availability / Adequacy
2.3.4.2. Human Resource / Staff Availability / Adequacy
2.3.4.3. Organization of Teams / People
2.3.4.4. Protocols / Policy / Procedure / Guideline Availability / Adequacy
3. C. Patient Characteristics
3.1. Age
3.1.1. _____ years
3.1.2. [checkbox] If <1, # of months
3.2. Sex
3.2.1. Male
3.2.2. Female
3.2.3. Unknown
3.3. Primary Diagnosis
3.3.1. Refer to section B. Pt Outcomes for chart
3.4. Reason for Transport
3.4.1. On Scene Response
3.4.2. Modified On Scene Response
3.4.3. Interfacility Response
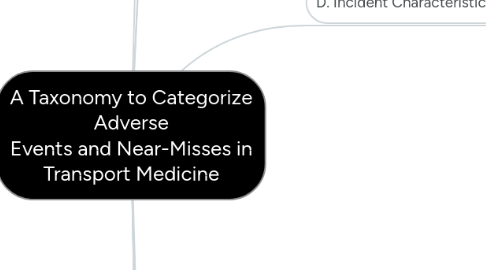
4. D. Incident Characteristics
4.1. Priority of Transport
4.1.1. Emergent
4.1.2. Urgent
4.1.3. Non-Urgent
4.1.4. Scheduled Transport
4.2. Phase of Treatment or Transfer
4.2.1. Pre-Admission to Ornge Service
4.2.2. Care on Admission, including Pre-Transfer Care from Sending
4.2.3. Transfer of Care to Receiving
4.2.4. Post-Discharge / Transfer
4.3. Care Setting
4.3.1. Hospital
4.3.2. Scene
4.3.3. Nursing Station
4.3.4. Airport
4.3.5. Medical Transport Service
4.3.5.1. Rotor Wing Aircraft
4.3.5.2. Fixed Wing Aircraft
4.3.5.3. Land Vehicle
4.3.6. Helipad / Heliport
4.3.7. Patient Holding Area
4.3.8. Commercial Airline
4.3.9. Base - Ornge
4.3.10. Base - Non Ornge
4.3.11. OCC
4.3.12. Ornge Head Office
4.3.13. Other
4.4. People Involved
4.4.1. Aviation
4.4.1.1. Air Traffic Control
4.4.1.2. Dispatch / Operations Control / Flight Following
4.4.1.3. Fueler
4.4.1.4. Maintenance Personnel / Engineer
4.4.1.5. Pilot / First Officer
4.4.1.6. Other Aviation Personnel
4.4.2. Patient Care
4.4.2.1. Dentist
4.4.2.2. Interpreter / Translator
4.4.2.3. Nurse
4.4.2.4. Nurse Practitioner
4.4.2.5. Occupational Therapist
4.4.2.6. Paramedic
4.4.2.7. Pharmacist
4.4.2.8. Physician
4.4.2.9. Physiotherapist
4.4.2.10. Physician Assistant
4.4.2.11. Pastoral Care Personnel
4.4.3. Partnered Organizations
4.4.3.1. CACC Personnel
4.4.3.2. Criticall Personnel
4.4.3.3. Local Health Integrated Network (LHIN) Personnel
4.4.3.4. MoH-EHS Personnel
4.4.3.5. Trillium Gift of Life Personnel
4.4.4. Medical Support
4.4.4.1. Assistant / Orderly
4.4.4.2. Biomedical Engineer
4.4.4.3. Imaging Technologist
4.4.4.4. Laboratory Technologist
4.4.4.5. Patient Transport / Retrieval Personnel
4.4.5. Public Safety
4.4.5.1. Fire Fighter
4.4.5.2. Liaison Officer
4.4.5.3. Police Officer
4.4.6. Others
4.4.6.1. ___________ (if not in list)
4.5. Person Reporting
4.5.1. Patient / Relative / Volunteer / Carer / Home Assistant
4.5.1.1. Patient
4.5.1.2. Another Patient
4.5.1.3. Relative / Guardian
4.5.1.4. Friend / Visitor
4.5.1.5. Volunteer
4.5.1.6. Carer / Home Aid / Assistant
4.5.1.7. Other
4.5.2. Please refer to c. Disciplines involved
5. E. Contributing Factors / Hazards
5.1. Staff Factors
5.1.1. Training
5.1.2. Orientation
5.1.3. Supervision / Assistance
5.1.4. Fatigue Management Strategies
5.1.5. Availability of Checklists / Protocols / Policies
5.1.6. Adequate Staff Numbers / Quality
5.2. Patient Factors
5.2.1. Adequate Care / Support Provision
5.2.2. Patient Education / Training Provision
5.2.3. Protocols / Decision Support Provision
5.2.4. Monitoring Equipment Provision
5.2.5. Medication Dispensing Aid Provision
5.3. Work / Environment Factors
5.3.1. Physical Environment / Infrastructure
5.3.2. Remote / Long Distance from Service
5.3.3. Environmental Risk Assessment / Safety Evaluation
5.3.4. Current Code / Specifications / Regulations
5.4. Organizational / Service Factors
5.4.1. Protocols / Policies / Procedure / Processes
5.4.2. Organizational Decisions / Culture
5.4.3. Discipline / Service
5.4.4. Organization of Teams
5.4.5. Emergency / Excavation / Disaster Plan
5.4.6. Resources / Workload
5.5. External Factors
5.5.1. Natural Environment
5.5.2. Products, Technology and Infrastructure
5.5.3. Services, Systems and Policies
5.5.4. Stakeholder Expectations
5.6. Mitigating Factors
5.6.1. Directed to Patient
5.6.1.1. Help Called For Patient
5.6.1.2. Management / Treatment / Care Undertaken
5.6.1.3. Patient Referred
5.6.1.4. Patient Education / Explanation
5.6.1.5. Apology
5.6.2. Directed to Staff
5.6.2.1. Good Supervision / Leadership
5.6.2.2. Good Team Work
5.6.2.3. Effective Communication
5.6.2.4. Relevant Person(s) Attended
5.6.2.5. Relevant Person(s) Educated
5.6.3. Directed to Organization
5.6.3.1. Effective Protocol Available
5.6.3.2. Product / Equipment / Device Management and Availability / Accessibility
5.6.3.3. Documentation Error Corrected
5.6.4. Directed to an Agent
5.6.4.1. Security / Physical Environment Measure
5.6.4.2. Infection Control Strategies Managed / Implemented
5.6.4.3. Therapeutic Agent Error Corrected
5.6.4.4. Equipment Usage Error Corrected
5.6.5. Other
5.6.5.1. Security / Physical Environment Measure
5.6.5.2. Infection Control Strategies Managed / Implemented
5.6.5.3. Therapeutic Agent Error Corrected
5.6.5.4. Equipment Usage Error Corrected
5.6.5.5. Good Luck / Chance
6. F. Error Recognition / Detection
6.1. Patient's Status Change
6.2. Machine / System / Environment / Change / Alarm
6.3. Count / Audit / Review
6.4. Proactive Risk Assessment
7. G. Organizational Outcomes
7.1. Property Damage
7.2. Increased Resource Allocation
7.3. Media Attention
7.4. Formal Complaint
7.5. Reputation Damaged
7.6. Legal Ramifications
8. H. Restitution / Rectifying Actions
8.1. Patient Related
8.1.1. Disease / Disorder Management
8.1.2. Management of Injury
8.1.3. Disability Management
8.1.4. Compensation
8.1.5. Open Disclosure / Apology
8.2. Organizational Related
8.2.1. Media Management / Public Relations
8.2.2. Complaint Management
8.2.3. Claims / Risk Management
8.2.4. Stress Debriefing / Staff Counselling
8.2.5. Local Notification and Restitution
8.2.6. Reconciliation / Mediation
8.2.7. Culture Change
8.2.8. Education / Training
9. I. Actions to Reduce Risk
9.1. Patient Factors
9.1.1. Refer to E
9.2. Staff Factors
9.2.1. Refer to E
9.3. Organizational / Environmental Factors
9.3.1. Physical Environment to Needs Matching
9.3.2. Access to Service Arrangements
9.3.3. Risk Assessment / Root Cause Analyses Performance
9.3.4. Current Code / Specifications / Regulations Being Met
9.3.5. Ready Access to Protocols / Policies / Decision Support Arranging
9.3.6. Leadership / Guidance Improvement
9.3.7. Staff to Tasks / Skills Matching
9.3.8. Safety Culture Improvement
9.4. Agent / Equipment Factors
9.4.1. Equipment Provision
9.4.2. Forcing Function
9.4.3. Regular Audits
