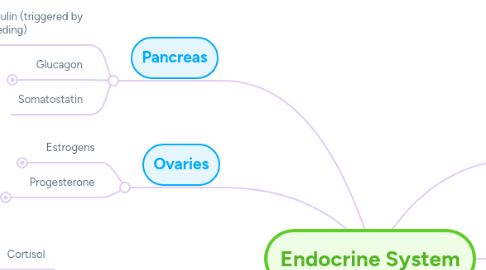
1. Pancreas
1.1. Insulin (triggered by feeding)
1.1.1. Glucose uptake and Glycogen deposition in the liver
1.1.2. Amino acids storage as protein in skeletal muscles
1.1.3. Triglyceride storage in fat
1.2. Glucagon
1.2.1. (triggered between meals)
1.2.1.1. Gluconeogenesis (Gluconeogenetic) and Glycogen breakdown (Glycogenolytic) in the liver
1.2.1.2. Lipolysis
1.2.2. (triggered with fasting - hypoglycemia)
1.2.2.1. Gluconeogenesis in the liver
1.3. Somatostatin
2. Ovaries
2.1. Estrogens
2.1.1. Control of Parturition/Changes
2.1.1.1. Further proliferation, expansion of endometrial (decidual) and myometrial layers
2.1.1.2. Further growth of vasculature, increased blood flow to deliver flow to placenta
2.1.1.3. Inhibition of LH and FSH secretion
2.1.1.4. Maternal behaviors
2.1.1.5. Increased blood flow to uterus → placenta
2.1.1.6. Increased fat deposition??
2.1.1.7. Uterine contraction
2.1.1.8. Increase contraction of smooth muscle (myometrium)
2.1.1.9. Increase prostaglandin (PGF2-alpha) production
2.1.1.10. Increase Oxytocin receptors
2.1.1.11. Increase gap junctions between myometrial cells
2.1.1.12. Prolactin (PRL) effects decreased during pregnancy by presence of E + P
2.1.1.13. At birth, decrease E+P : increase PRL action
2.1.2. In relation to Bone
2.1.2.1. Inhibits Osteoclasts
2.1.3. Effects at Puberty
2.1.3.1. E: (reproductive tract): growth and development of uterus, vagina, fallopian tubes
2.1.3.2. E: (secondary sex characteristics)
2.1.3.2.1. female pattern of fat deposition
2.1.3.2.2. breast development
2.1.3.2.3. development of external genitalia
2.1.3.3. E: (bone) growth, epiphyseal closure
2.1.4. Effects at Adults
2.1.4.1. E: (reproductive tract in follicular phase)
2.1.4.1.1. maturation of vaginal epithelium
2.1.4.1.2. endometrial proliferation - vessels and glands
2.1.4.1.3. clear cervical mucus (mucus allows sperm to go up through cervix to penetrate and be able to get fertilized)
2.1.4.1.4. maintain P receptors
2.1.4.2. E: (brain)
2.1.4.2.1. effects on brain development
2.1.4.2.2. effects on serotonin, mood
2.1.4.2.3. may be protective effects on neuron response to injury
2.1.4.3. E: (CV)
2.1.4.3.1. lowers BP through vasodilation in some tissues greatest effect on uterine blood flow
2.1.4.3.2. may have protective effects
2.1.4.4. E: (liver)
2.1.4.4.1. increase production of SHBG, TBG, CBG, angiotensinogen
2.1.4.4.2. decrease cholesterol, LDL production
2.1.4.4.3. increase HDL production
2.2. Progesterone
2.2.1. Control of Parturition/Changes
2.2.1.1. Decreases uterine contractility
2.2.1.2. Inhibition of LH and FSH secretion
2.2.1.3. Increased body temperature
2.2.1.4. Maternal behaviors
2.2.1.5. Increased fat deposition??
2.2.1.6. Uterine quiescence
2.2.1.7. MUST have P to maintain pregnancy,prevent spontaneous abortion (↑ P)
2.2.1.8. Decreases estrogen and oxytocin receptors in myometrium
2.2.1.9. Prolactin (PRL) effects decreased during pregnancy by presence of E + P
2.2.1.10. At birth, decrease E+P : increase PRL action
2.2.2. Effects at Adults
2.2.2.1. P: (reproductive tract in luteal phase)
2.2.2.1.1. secretion of endometrial and f. tube glands
2.2.2.1.2. decreased myometrial estrogen receptor
2.2.2.1.3. thick cervical mucous (make it hard for bacteria to get through/protective effect)
3. Adrenal Gland
3.1. Cortisol
3.1.1. In relation to Glucose and Metabolism
3.1.1.1. (triggered with fasting - hypoglycemia)
3.1.1.1.1. Glycogen storage in the liver
3.1.1.1.2. Proteins breakdown in skeletal muscles
3.1.1.1.3. Amino acids used for Gluconeogenesis
3.1.1.1.4. Promote lipolysis,
3.1.1.1.5. Ketone production (with starvation, suppress glucagon & ketones are fuel source)
3.1.2. In relation to Bone
3.1.2.1. Causes osteoblasts apoptosis, therefore, it able to turn off osteoblasts (not much bone formation)
3.2. Epinephrine
3.2.1. (triggered between meals)
3.2.1.1. Decrease Glucose uptake (indirectly opposes insulin actions)
3.2.1.2. Gluconeogenesis and Glycogen breakdown in the liver.
3.2.1.3. Glycogen breakdown in skeletal muscles
3.2.1.4. Glycogen breakdown in skeletal muscles
3.2.1.5. Lipolysis
3.2.2. (triggered with fasting - hypoglycemia)
3.2.2.1. Gluconeogenesis in the liver
3.2.2.2. Lipolysis
3.3. Norepinephrine
3.4. Aldosterone
3.5. Adrenal Androgens
4. Pituitary Gland
4.1. Anterior Pituitary
4.1.1. FSH
4.1.1.1. Granulosa Cells: aromatase activity (converts A → E2)
4.1.1.2. Granulosa Cells: nutrient production
4.1.1.3. Granulosa Cells: inhibin secretion (keeps FSH low)
4.1.2. LH
4.1.2.1. Thecal cells: Synthesis of testosterone.
4.1.2.2. Luteal cells: Increase production of progesterone (minor part of P → A → E)
4.1.2.3. Luteal cells: Controls aromatase : Androgens → Estrogen
4.1.3. TSH
4.1.4. GH
4.1.4.1. In relation to Glucose and Metabolism
4.1.4.1.1. Decreased insulin sensitivity
4.1.4.1.2. Protein synthesis
4.1.4.1.3. Lipolysis
4.1.5. Prolactin
4.2. Posterior Pituitary
4.2.1. Oxytocin
4.2.1.1. Oxytocin → uterine contractions → cervical stretch → oxytocin → uterine contractions → → DELIVERY (Positive FEEDBACK)
4.2.1.2. Suckling: Oxytocin milk ejection (myoepithelial cell contraction)
4.2.2. Vasopressin
5. Hypothalamus
5.1. Releasing Hormones
5.1.1. GnRH
5.1.2. CRH
5.1.3. TRH
5.1.4. GHRH
5.2. Inhibitory Hormones
5.2.1. PIF (Prolactin Inhibitory Factor)
5.2.2. Dopamine
5.2.3. Oxytocin
5.2.4. Vasopressin
5.2.5. Somatostatin
6. Thyroid Gland
6.1. T3
6.2. T4
6.3. Calcitonin
6.3.1. In relation to Bone
6.3.1.1. Inhibits Osteoclasts
7. Parathyroid Gland
7.1. PTH
7.1.1. In relation to Bone
7.1.1.1. Stimulates Osteoclasts
8. Testes
8.1. Testosterone
8.1.1. Testosterone (T) and DHT actions
8.1.1.1. Fetus
8.1.1.1.1. T: Development of epididymis, vas deferens, seminal vesicles (INTERNAL)
8.1.1.1.2. DHT: development of penis, scrotum, urethra
8.1.1.1.3. DHT>T: development of prostate, descent of testes (In some cases, Same for testosterone with high concentration)
8.1.1.2. Puberty
8.1.1.2.1. T: seminal vesicles, growth of musculature of larynx, bone growth
8.1.1.2.2. DHT: growth of prostate, male pattern hair growth
8.1.1.2.3. DHT>T: growth of penis, activity of sebaceous and sweat glands (Also can be seen with high testosterone concentration at puberty)
8.1.1.2.4. E: epiphyseal closure (Testosterone aromatized to Estrogen (E))
8.1.1.2.5. Low 5a reductase activity (Converts T to DHT) – missing DHT actions, external genitalia undeveloped until puberty
8.1.1.2.6. In some cases reduction of 5a reductase activity reduction might be a helpful therapy for men with benign prostate hypertrophy
8.1.1.3. Adults
8.1.1.3.1. T: sperm production, inhibit breast development (by inhibiting estradiol)
8.1.1.3.2. T: ↑ VLDL, ↑ LDL, ↓ HDL (Men's tend to have not as good LDL/HDL ratio as premenopausal women, because the effect of testosterone)
8.1.1.3.3. T: male body build- ↑ muscle mass, ↑ trunk body fat
8.1.1.3.4. T: ↑ erythropoietin (Important for red blood cells production. Men's tend to have higher RBC counts)
8.1.1.3.5. T: maintain bone mass
8.1.1.3.6. DHT,T: maintain external genitalia and accessory sex organ function
8.1.1.3.7. DHT >T and E: male pattern of gonadotropin secretion (low amplitude, slow pulses)

