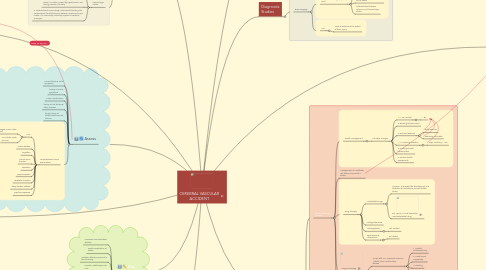
1. Plan
1.1. maximize communication abilities
1.2. avoid complication of stroke
1.3. maintain effective personal & family coping
1.4. maintain stable/improved LOC
1.5. Maximum physical functioning
1.6. maximum self-care abilities & skills
1.7. stable body functions (bladder control, etc.)
2. Monitor
2.1. Respiratory System
2.1.1. atelectasis
2.1.2. aspiration pneumonia
2.1.3. airway obstruction
2.1.4. endotracheal intubation & mechanical ventilation requirement
2.1.5. ineffective airway clearence
2.2. Neurological System
2.2.1. extension of stroke
2.2.2. increased intracranial pressure
2.2.3. vasospasm
2.2.4. Glasgow Coma Scale (GCS)
2.2.5. NIH Stroke Scale (NIHSS)
2.3. Cardiovascular System
2.3.1. vital signs
2.3.2. cardiac rhythm
2.3.3. intake & output
2.3.4. fluid intake
2.3.5. crackles & ronchi (pulmonary congestion)
2.3.6. murmurs or S3/S4
2.4. impaired physical mobility
2.5. impaired verbal communication
2.6. unilateral neglect
2.7. impaired urinary elimination
2.8. ineffective cerebral tissue perfusion
2.9. perceptual deficits
2.10. Warning Siigns
2.10.1. sudden weakness, paralysis or numbness of face, arm, leg; especially unilaterally
2.10.2. sudden dimness or loss of vision
2.10.3. sudden confusion, loss of speech or difficulty speaking or understanding speech
2.10.4. unexplained sudden dizziness, unsteadiness, loss of balance or coordination
2.10.5. sudden severe or unusual headache
3. Assess
3.1. current illness & initial symptoms
3.2. history of similar symptoms
3.3. current medications
3.4. history of risk factors & other illnesses
3.5. family history of stroke/cardiovascular disease
3.6. comprehensive neuro examination
3.6.1. LOC
3.6.1.1. Glasgow Coma Scale (GCS)
3.6.1.2. NIH Stroke Scale (NIHSS)
3.6.2. motor abilities
3.6.3. cognition
3.6.4. cranial nerve fucntion
3.6.5. sensation
3.6.6. proprioception
3.6.7. cerebellar function
3.6.8. deep tendon reflexes
3.6.9. pupillary response
4. What Is Stroke?
4.1. Stroke occurs when ischemia or hemorrhage into brain results in death of brain cells. It is the 3rd most common cause of death in Canada.
4.2. Ischemic Stroke
4.2.1. Inadequate blood flow to brain from partial/complete occlusion of artery (80% of all strokes)
4.2.2. 1. Transient Ischemic Attack: transient episode of neurological dysfunction caused by focal brain, spinal cord or retinal ischemia
4.2.3. 2. Thrombotic Stroke: related to blood vessel injury & formation of blood clot -> narrow blood vessel
4.2.4. 3. Embolic Stroke: embolus lodges in & occlude cerebral artery -> infarction & edema of area supplied by that vessel
4.3. Hemorrhagic Stroke
4.3.1. From bleeding into brain tissue (intracerebral) or into subarachnoid space or ventricles (15% of all strokes)
4.3.2. 1. Intracerebral Hemorrhage: rupture of a vessel. It is often caused by hypertension and during periods of activity.
4.3.3. 2. Subarachnoid Hemorrhage: intracranial bleeding into cerebrospinal fluid-filled space between arachnoid & pia matter. It is commonly caused by rupture of cerebral aneurysm.
5. Implement
5.1. Respiratory System
5.1.1. airway potency & function
5.1.2. oxygenation
5.1.3. suctioning
5.1.4. patient mobility
5.1.5. positioning to prevent aspiration
5.1.6. deep breathing
5.2. Neurological Ssystem
5.2.1. closely monitor changes suggesting stroke, increased ICP, vasospasm or recovery from stroke symptoms
5.3. Cardiovascular System
5.3.1. maintain homeostasis/cardiac reserves
5.3.2. keep patient moving to prevent vein thrombosis
5.4. Musculoskeletal System
5.4.1. prevention of joint contractions & muscle atrophy
5.4.2. range of motion exercise & positioning
5.5. Integumentary System
5.5.1. monitor loss of sensation, decreased circulation & immobility
5.5.2. hygiene & emollient application
5.5.3. pressure relief
5.6. Bowel Management
5.6.1. stool softeners/fibres (psyllium)
5.6.2. avoid in-dwelling catheters
6. Health Promotion
6.1. Coping
6.1.1. emotionally & socially
6.1.2. changing roles & responsibilities
6.1.3. social service referral
6.2. Ambulatory & Home Care
6.2.1. education
6.2.1.1. medication
6.2.1.2. nutrition
6.2.1.2.1. swallowing/gag reflex
6.2.1.3. mobility
6.2.1.4. exercises
6.2.2. demonstration
6.2.3. practice
6.2.4. evaluation of self-care skills
7. Research Article
7.1. Barriers to cardiovascular disease healthcare
7.1.1. Patient
7.1.1.1. availability, access & costs
7.1.1.2. knowledge, beliefs, memory
7.1.2. Healthcare Provider
7.1.2.1. knowledge
7.1.2.2. attitudes/behaviour
7.1.3. Health System & Policy
7.1.3.1. financing system
7.1.3.2. medical products & technologies
7.1.3.3. leadership/governance
7.1.3.4. health workforce
7.1.3.5. service delivery
7.1.3.6. Health information system & research
7.2. Resource effective strategies to prevent and treat cardiovascular disease
7.2.1. tobacco control
7.2.2. simplified screening & management algorithms for those at risk
7.2.3. availability and affordability of treatment regimens
7.2.4. simplified delivery of healthcare through task-sharing
7.2.5. optimizing self-management
8. Collaborative Care
8.1. Stroke Prevention Therapy
8.1.1. Health Management
8.1.1.1. Life style changes
8.1.1.1.1. 1. BP Control
8.1.1.1.2. 2. Blood gluclose control
8.1.1.1.3. 3. Diet and Exercise
8.1.1.1.4. 4. Smoking cessation
8.1.1.1.5. 5. Limiting alcohol consumption
8.1.1.1.6. 6. Routine health assessments
8.1.2. Management of modifiable risk factors to prevent a stroke
8.1.3. Drug Therapy
8.1.3.1. Antiplatelet Drugs
8.1.3.1.1. Purpose: To prevent the development of a thrombus or embolus to prevent further stroke
8.1.3.1.2. Ex) Aspirin = most frequently used antiplatelet drug
8.1.3.2. Antihypertensives
8.1.3.3. Anticoagulants
8.1.3.3.1. Ex) Warfarin
8.1.3.4. Lipid-lowering Medications
8.1.3.4.1. Ex) Statins
8.1.4. Surgical Therapy
8.1.4.1. For pt with TIAs (Transient Ischemic Attacks) from carotid artery disease
8.1.4.1.1. 1. Carotid endarterectomy
8.1.4.1.2. 2. Transluminal angioplasty
8.1.4.1.3. 3. Stenting
8.1.4.1.4. 4. Extracranial-to-intracranial artery bypass
8.1.5. A summary of the above preventive measures
8.2. Acute Care
8.2.1. Focus is on (1) preserving life, (2) preventing further brain damage, (3) reducing disability
8.2.1.1. Acute Care for Ischemic Stroke
8.2.1.1.1. Drug Therapy
8.2.1.2. Acute Care for Hemorrhagic Stroke
8.2.1.2.1. Drug Therapy
8.3. Rehabilitation Care
8.3.1. Focus is on (1) lessening disability, (2) attaining optimal function
8.3.1.1. Inpatient rehabilitation intervention
8.3.1.1.1. Evidence-based mobility intervention was associated with improvements in mobility achievement, discharge functional outcomes, and quality of life for patients with hemorrhagic stroke. Activities in the intervention included progressive activities to improve coordination, strength, and range of motion. (Rand & Darbinian, 2015)
8.3.1.2. Outpatient therapy
8.3.1.3. Home care-based rehabilitation
8.3.1.3.1. Neurologic Music Therapy targeting language rehabilitation
9. Risk Factors
9.1. Modifiable Risk Factors
9.1.1. Hypertension
9.1.1.1. Hypertension is the most important modifiable risk factor that is often undetected and inadequately treated. Stroke risk can be significantly reduced through the adequate treatment and early diagnosis of hypertension.
9.1.2. Heart Disease
9.1.3. Diabetes Mellitus
9.1.4. Increased Serum Cholesterol
9.1.5. Obesity
9.1.6. Drug Abuse
9.1.7. Alcohol
9.1.8. Physical Inactivity
9.1.9. Smoking
9.2. Non-Modifiable Risk Factors
9.2.1. Age
9.2.1.1. Stroke risk increases with age, doubling each decade after 55 years of age
9.2.2. Gender
9.2.2.1. Strokes are more common in men, but more women die from stroke than men
9.2.3. Ethnicity and Race
9.2.4. Heredity/Family History
9.2.5. Low Birth Weight
10. Clinical Manifestations
10.1. Motor Deficits
10.1.1. Impairment of (1) mobility; (2) respiratory function; (3) swallowing and speech; (4) gag reflex; (5) self-care abilities
10.2. Communications
10.2.1. Aphasia
10.2.1.1. Total loss of comprehension and use of language
10.2.1.1.1. Due to damages to the dominant hemisphere of the brain
10.2.2. Dysphasia
10.2.2.1. Difficulty related to the comprehension or use of language
10.2.2.1.1. Due to partial disruption or loss
10.2.3. Dysarthria
10.2.3.1. A disturbance in the muscular control of speech -> Impaired pronunciation, articulation, and/or phonation
10.3. Affect
10.3.1. Difficulty controlling their emotions
10.3.2. Depression and frustration associated with loss of function
10.4. Intellectual Function
10.4.1. Impaired memory and/or judgment
10.5. Spatial-perceptual Alterations
10.5.1. Anosognosia
10.5.1.1. Deny their illnesses or their own body parts
10.5.2. Homonymous Hemianopsia
10.5.2.1. Blindness occurs in the same half of the visual fields of both eyes -> Difficulties with spatial orientation
10.5.3. Agnosia
10.5.3.1. Inability to recognize an object by sight, touch, or hearing
10.5.3.1.1. In the video, she not only has difficulties in visually recognizing her glasses but also displays spatial orientation impairment.
10.5.4. Apraxia
10.5.4.1. Inability to carry out learned sequential movements on command
10.6. Urinary and Bowel Elimination
10.6.1. Experiences frequency, urgency, and incontinence usually early on and temporarily
11. Right-Brain Damage Vs. Left-Brain Damage
12. Diagnostic Studies
12.1. Brain Imaging
12.1.1. Computed Tomography (CT) Scan
12.1.1.1. Primary diagnostic test used after a stroke
12.1.1.2. Indicates the size and location of the lesion
12.1.1.3. Differentiates between ischemic and hemorrhagic stroke
12.1.2. MRI
12.1.2.1. Used to determine the extent of brain injury

