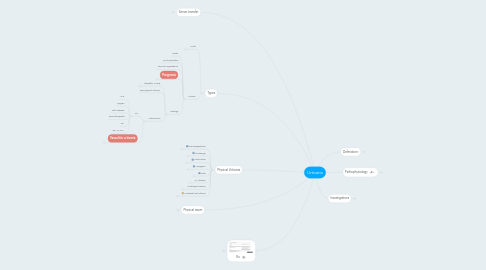
1. Types
1.1. Acute
1.1.1. <6wks
1.1.2. 20% of population
1.1.3. Ax
1.1.3.1. Food
1.1.3.2. Drug
1.1.3.3. Infections
1.1.3.3.1. Viral illness
1.1.3.3.2. Mycoplasma
1.1.3.3.3. Bacterial
1.1.3.3.4. Parasites
1.1.3.4. contact
1.1.3.4.1. Latex
1.1.3.4.2. Food
1.1.3.5. Insect
1.1.4. Prognosis
1.1.4.1. 30%--->chronic urticaria
1.2. Chronic
1.2.1. >6wks
1.2.2. 1% of population
1.2.3. 40% a/w angioedema
1.2.4. Prognosis
1.2.4.1. 50% will resolve w/in 1 year
1.2.4.2. 20% will persist >10 years
1.2.5. Etiology
1.2.5.1. Idiopathic in 80%
1.2.5.1.1. a/w autoantibodies
1.2.5.2. 20% physical urticaria
1.2.5.3. Autoimmune
1.2.5.3.1. 2/2
1.2.5.3.2. Vasculitis urticaria
2. Physical Urticaria
2.1. Dermatographism
2.1.1. The most common
2.1.2. Less pruritic
2.1.3. Linear rash after striking the skin with tongue depressor and may last for 30 mins
2.1.4. Types
2.1.4.1. Simple
2.1.4.1.1. The most common
2.1.4.1.2. Dermatographea
2.1.4.1.3. Less pruritic
2.1.4.2. Symptomatic dermatographism
2.1.4.2.1. Very pruritic
2.1.4.2.2. Occur in pressure area
2.1.4.3. Red, white or follicular dermatographism
2.1.5. Pathogenesis
2.1.5.1. Serum transferred
2.1.5.2. Maybe baseline elevation of histamine
2.1.6. A/W
2.1.6.1. Mastocytosis
2.1.6.2. Solar Urticaria
2.1.6.3. Abx use
2.1.6.4. Stress
2.2. Cholinergic
2.2.1. Characteristics
2.2.1.1. Small hives 1-3mm w/ surrounding erythema (like SPT)
2.2.2. Trigger
2.2.2.1. Passive heating
2.2.2.1.1. Hot shower
2.2.2.2. Active heating
2.2.2.2.1. Exercise
2.2.2.3. Sweating
2.2.2.4. Anxiety
2.2.3. Severity
2.2.3.1. Mild to life threatening
2.2.4. Provocative testing
2.2.4.1. Exercise
2.2.4.2. Hot water emersion (41C)
2.2.4.2.1. bring up the body temperature by 0.7C
2.2.4.3. Methacholine intracutaneous testing
2.2.4.3.1. 0.01mg/1ml methacholine + 0.1ml of normal saline
2.2.4.4. But negative predictive value of these are unknown
2.2.5. 3 different pathophysiological mechanism
2.2.5.1. Sensitivity to autologus sweat
2.2.5.1.1. Antibody mediated
2.2.5.1.2. Direct degranulation of basophils
2.2.5.2. Exaggerated cutaneous response to acetylcholine
2.2.5.3. Neurogenic reflex
2.2.5.3.1. Altered central perception of temperature changes
2.2.6. May have extracutenous manifestations
2.2.6.1. Salivation
2.2.6.2. Lacrimation
2.2.6.3. Bronchospasm
2.2.6.4. Diarrhea
2.2.7. Rx
2.2.7.1. Atarax (hydrozyxin)
2.2.7.1.1. It has anticholinergic effect
2.3. Cold induce
2.3.1. Ax
2.3.1.1. Primary
2.3.1.1.1. Aquired
2.3.1.1.2. Familial
2.3.1.2. Secondary
2.3.1.2.1. Infections
2.3.1.2.2. Vasculitis
2.3.1.2.3. Cold dependent immunoglobulin diseases
2.3.1.3. Localized cold urticaria
2.3.1.3.1. two types
2.3.1.4. It is imp to differentiate it from familial cold autoinflammatory syndrome
2.3.1.4.1. It is part of the cryopyroin associated periodic syndrome
2.3.1.4.2. Non urticarial rash
2.3.2. Dx by ice cube test placed for 10 mins
2.3.2.1. -ve ice cube test in]
2.3.2.1.1. systemic cold urticaria
2.3.2.1.2. Cold induce cholenergic urticaria
2.3.2.1.3. Cold dependent dermatographism
2.3.2.1.4. FCAS
2.3.2.1.5. PLAID (phospholipase Cγ2-Associated Antibody Deficiency and Immune Dysregulation)
2.3.3. Rx
2.3.3.1. If angioedema (mucosal membrane), epipen, swimming in public places. Avoid submersion of the body above waist line.
2.4. Aquagenic
2.4.1. extremely rare
2.4.1.1. reported on 50 people
2.4.2. Pinpoint hives (similar to cholinergic, 1-3mm)
2.4.3. independent of water temperature
2.4.4. Dx
2.4.4.1. placing wet compress such as wash cloth at 35C on the upper body for 15-30 min
2.4.5. May have systemic symptoms
2.4.5.1. headache
2.4.5.2. Respiratory symptoms
2.5. Solar
2.5.1. w/in min of sun exposure
2.5.2. Dx
2.5.2.1. Exposure to different wave lengths
2.5.3. DDx
2.5.3.1. Phototoxic & photo allergic drug eruptions
2.5.3.2. polymorphous light eruption
2.5.3.2.1. Delay hypersensitivity reaction
2.5.3.2.2. Component of the skin gets alter with exposure to ultraviolate radiation
2.5.3.2.3. The most common photodermatosis
2.5.3.2.4. Lack of systemic symptoms
2.5.3.2.5. Rash is itchy and painful
2.5.3.3. CTD
2.5.4. UVA might be effective
2.5.4.1. Thickening the skin
2.5.5. Chromophore
2.5.5.1. Substance that are circulated in the blood that got activated by light and sIgE will bind to it
2.6. 6) Vibratory
2.6.1. Dx
2.6.1.1. Vortex mixer
2.7. 7) Delayed Pressure
2.7.1. typically developed 6-8hrs later
2.7.1.1. can be 24hrs
2.7.1.2. rarely within 1hrs
2.7.2. Pathology is different than other CU
2.7.2.1. inflammatory cells predominant (neutrophils & eosinophil) instead of mast cell.
2.7.2.2. May a/w inc IL-6 and TNF
2.7.2.2.1. low grade fever
2.7.2.2.2. Malaise
2.7.3. Less reposnsive to anti-histamines--Make sense!
2.7.3.1. Rx. Singulair and steroid
2.7.4. Dx.
2.7.4.1. suspend 15ibs weight over pt shoulder for 10-15min
2.7.4.1.1. positive response
2.8. 8) Localized heat urticaria
2.8.1. Apply tube with that contain hot water (45C) to arm for 5 minutes
3. Serum transfer
3.1. Passive transfer by serum
3.1.1. Cold
3.1.1.1. IgG, IgM, IgE or cryoglobulin
3.1.2. Dermatographism
3.1.2.1. IgE
3.1.3. Solar
3.1.3.1. Type 1 or Type 4 allergic reaction
4. Physical exam
4.1. Urticarial vasculitis
4.1.1. Last >24hrs
4.1.2. Painful not itchy
4.1.3. Hyperpigmentation
4.1.4. Surrounding petechia
4.2. Dermatographism
4.3. Thyroid for dysregulation
4.4. LAP and liver
4.4.1. for CLL and hepatitis (HBV & HCV)
4.4.1.1. A/W cryoglobulinemia-->cold induce urticaria and urticarial vasculitis
4.5. if hyper pigmented lesion
4.5.1. Strike the skin to demonstrate if darier sign present-->cutaneous mastocytosis-->send baseline tryptase
5. Rx.
5.1. Counselling
5.1.1. Not serious yet troblesome
5.2. drugs
5.2.1. Second generation H1 blockers
5.2.1.1. Cetrizine (Reactin)
5.2.1.1.1. 10mg OD-->BID-->20mgBID
5.2.1.2. Levocetrizine(Xyzal)
5.2.1.2.1. dosing 5-->10-->20mg QHS
5.2.1.3. Desoloratadine (Aerius)
5.2.1.3.1. Same dosing as levocitrizine
5.2.1.4. Loratadine (Claritin)
5.2.1.5. Fexofenadine (allegra)
5.2.1.5.1. 20/60/120/240mg BID
5.2.2. Increase dose of 2nd gen to X4 the regular dose
5.2.3. Leukotriene antagonist
5.2.3.1. Montelukast
5.2.3.2. Zafirolukast
5.2.4. Doxepine
5.2.4.1. TCA with H1 and H2 blocking activity
5.3. Avoid
5.3.1. NSAIDs
5.4. Third line (last resort)
5.4.1. Colchicine
5.4.2. Sulphasalazine
5.4.3. Dapson
6. Definiation:
6.1. Urticaria
6.1.1. Raised
6.1.2. Pruritic
6.1.3. Erythematous
6.1.4. Transient
6.1.4.1. <24hrs in same spot
7. Pathophysiology
7.1. Early phase
7.1.1. Vasoactive mediators
7.1.1.1. Immediate
7.1.1.1.1. Histamine
7.1.1.2. Membrane phospholipids
7.1.1.2.1. Leukotrienes
7.1.1.2.2. Prtostaglandins
7.1.2. Vasodilatation
7.1.3. In urticaria
7.1.3.1. superficial dermis
7.1.4. In angioedema
7.1.4.1. deep dermis
7.2. Late phase
7.2.1. 4-8hrs
7.2.2. Cytokines
7.2.2.1. TNF-a
7.2.2.2. IL-4
7.2.2.2.1. Th2
7.2.2.2.2. Switch to IgE
7.2.2.3. IL-5
7.2.2.3.1. Eosinophillic recruiter
7.2.2.3.2. IgA switching in the gut
7.2.3. Inflammatory cells
7.2.3.1. Acute urticaria
7.2.3.1.1. Rare infiltrate
7.2.3.2. Chronic Urticaria
7.2.3.2.1. Perivascular
7.2.3.3. So pathology is different between the two! yet biopsy is rarely needed.
7.3. CSU (chronic sponteous urticaria)
7.3.1. You may see basopenia
7.3.2. Two types of basophils
7.3.2.1. IgE responser
7.3.2.2. Non-IgE responser
8. Investigations
8.1. Acute Urticaria
8.1.1. Skin test +/- sIgE based on hx.
8.2. Chronic urticaria
8.2.1. In unremarkable hx and px
8.2.1.1. Consider CBC/diff/ESR/CRP/LFT/TSH
8.2.2. Not routinely recommended
8.2.2.1. anti-thyroid antibodies
8.2.2.2. Anti-FcRa or anti-IgE Fc
8.2.2.3. Skin test for food, inhalants etc..
8.2.3. Case by case
8.2.3.1. biopsy if suspected vasculitis
8.2.3.2. C1 estrase assay if isolated angioedema, C4
8.2.3.3. Cryglobulinemeia
8.2.3.3.1. HCV
8.2.3.4. Autoimmune work-up (ANA, anti-DsDNA, RF, C3,C4 etc..)
