1. Medical Emergencies
1.1. Management of Cardiac Arrest
1.1.1. Basic Life Support
1.1.1.1. Automated external defibrillator
1.1.1.1.1. Heimlich Maneuver
1.1.1.2. Advance Life Support
1.1.1.2.1. continued Chest compressions & ventilation
1.1.2. Acute Respiratory Distress Syndrome
1.1.2.1. Phases: Exudative, Proliferative, Fibrotic
1.1.2.1.1. Treatment: Mechanical Ventilatory Support (low tidal volumes combined with PEEP) and Ancillary Therapies (IV fluids as needed and tissue O2 delivery, acid-base status and arterial pressure
1.1.3. Bioterrorism
1.1.3.1. Microbial Bioterrorism
1.1.3.1.1. genetic alteration of microbes, creation of fine particle aerosols, chemical treatment, alteration of host range
1.1.3.1.2. Category A agents: Anthrax, Plague, Smallpox, Tularemia, Viral Hemorrhagic fevers, Botulinum Toxin
2. Hematology and Oncology
2.1. Examination of Blood Smears and Bone Marrow
2.1.1. Blood Smears
2.1.1.1. Erythrocyte (RBC) Morphology
2.1.1.1.1. RBC Inclusions
2.1.2. Bone Marrow
2.1.2.1. Indications: Aspiration, Special tests, Biopsy
2.1.2.1.1. Interpretation: Cellularity, Erythroid:Granulocytic (E:G) Ratio
2.2. Red Blood Cell Disorders
2.2.1. Hypoproliferative Anemias
2.2.2. Maturation Disorders
2.2.3. Anemia due to RBC destruction or Acute Blood Loss
2.2.3.1. Blood loss: Trauma, GI Hemorrhage, Genitourinary sources, internal bleeding
2.2.3.1.1. Hemolysis:Intracellular RBC abnormalities, G6PD deficiency,Sickle cell anemia, Membrane abnormalities, Immunohemolytic Anemia, Mechanical trauma, Direct Toxic effect, Hypersplenism
2.2.4. Anemia Specific Disorders
2.2.4.1. Iron deficiency, Folate deficiency, Vitamin B12 deficiency, Anemia of chronic disease, Sickle cell anemia, Thalassemia, Aplastic Anemia, Autoimmune hemolysis, G6PD deficiency
2.2.5. Treatment: Transfusion therapy with packed RBC, Hct should increase 3-4% or Hb by 10g/L
2.3. Leukocytosis and Leukopenia
2.3.1. Leukocytosis
2.3.1.1. Neutrophilia
2.3.1.1.1. Leukemoid Reaction
2.3.2. Leukopenia
2.3.2.1. Neutropenia
2.3.2.1.1. Lymphopenia
2.4. Bleeding and Thrombotic Disorders
2.4.1. Platelet Disorders
2.4.1.1. Thrombocytopenia
2.4.1.1.1. Pseudothrombocytopenia
2.4.2. Hemostatic Disorders due to Blood vessel wall defects
2.4.3. Disorders of Blood Coagulation
2.4.3.1. Congenital Disorders: Hemophilia A, Hemophilia B, von Willebrand disease
2.4.3.2. Acquired Disorders: Vitamin K deficiency, Liver disease, DIC, fibrinogen deficiency
2.4.3.3. For refractory patients: Splenectomy, danazol, vincristine, cyclophosphamide, fludarabine
2.4.4. Thrombotic Disorders
2.4.4.1. Hypercoagulable State
2.4.4.1.1. Treatment: Anticoagulant agents, Fibrinolytic agents, Antiplatelet agents
2.5. Myeloid Leukemias, Myelodysplasia, Myeloproliferative Syndromes
2.5.1. Acute Myeloid Leukemia (AML)
2.5.1.1. Chronic Myeloid Leukemia (CML)
2.5.1.2. Myelodysplastic Syndromes (MDS)
2.5.1.3. Myeloproliferative Syndromes
2.5.1.3.1. Polycythemia vera
2.5.1.3.2. Idiopathic Myelofibrosis
2.5.1.3.3. Essential thrombocytosis
2.6. Lymphoid Malignancies
2.6.1. Chronic lymphoid leukemias
2.6.1.1. Chronic Lymphocytic Leukemia
2.6.2. Indolent lymphoma
2.6.2.1. Follicular Lymphoma
2.6.3. Aggressive lymphoma
2.6.4. Acute lymphoid leukemias/lymphomas
2.6.4.1. Acute Lymphoblastic Leukemia and Lymphoblastic lymphoma
2.6.4.2. Burkitt's Lymphoma/Leukemia
2.6.4.3. Adult T cell Leukemia/lymphoma
2.6.5. Plasma cell disorders
2.6.5.1. Multiple Myeloma
2.6.6. Hodgkin's Disease
3. Infectious Diseases
3.1. Diagnosis of Infectious Diseases
3.1.1. Microscopy
3.1.1.1. Wet mounts
3.1.1.2. Stains
3.1.1.2.1. Gram's stain
3.1.2. Macroscopic Antigen Detection
3.1.3. Culture
3.1.4. Serology
3.1.5. Nucleic Acid Probes
3.1.6. Susceptibility Testing
3.1.7. Fecal Samples for Intestinal parasites
3.1.8. Blood Smears for Blood and Tissue Parasites
3.2. Antibacterial Therapy
3.2.1. Mechanism of Drug Action
3.2.1.1. Inhibition of cell-wall synthesis (Penicillin, cephalosporins,carbapenems, vancomycin,bacitracin)
3.2.1.2. Inhibition of protein synthesis (Macrolides, lincosamides, chloramphenicol, tetracycline, aminoglycosides, muciprocin, streptogramins, linezolid)
3.2.1.3. Inhibition of bacterial metabolism (Sulfonamides and trimethoprim)
3.2.1.4. Inhibition of nucleic acid synthesis or activity (Rifampin, Nitrofurantoin, Metronidazole)
3.2.2. Mechanism of Antibacterial Resistance
3.2.3. Pharmacokinetics of Antibiotics
3.2.3.1. Absorption
3.2.3.2. Distribution
3.2.3.3. Metabolism
3.2.3.4. Elimination
3.2.4. Principles of Antibacterial chemotherapy
3.2.4.1. Pharmacokinetic-pharmacodynamic profile
3.2.4.1.1. Concentration-dependent antibiotics
3.2.4.1.2. Time-dependent antibiotics
3.2.5. Choice of Antibacterial agents
3.2.6. Adverse Reactions
3.2.7. Drug interactions
3.3. Sexually Transmitted and Reproductive Tract Infections
3.3.1. Specific Syndromes
3.3.1.1. Urethritis in Men
3.3.1.2. Epididymitis
3.3.1.3. Urethritis in Women (Urethral syndrome)
3.3.1.4. Vulvovaginal Infections
3.3.1.5. Mucopurulent Cervicitis
3.3.1.6. Pelvic Inflammatory Disease (PID)
3.3.1.7. Ulcerative Genital Lesions
3.3.1.8. Proctitis, Proctocolitis, Enterocolitis & Entiritis
3.3.2. Individual Pathogens
3.3.2.1. Gonorrhea
3.3.2.2. Chlamydia trachomatis infections
3.3.2.3. Mycoplasmas infections
3.3.2.4. Syphilis
3.3.2.5. Herpes Simplex Virus Infections
3.3.2.6. Chancroid (Haemophilus Ducreyi infection)
3.3.2.7. Donovanosis (Klebsiella granulomatis infection)
3.3.2.8. Human Papillomavirus infections
3.4. Infections of the Skin, Soft Tissues, Joints and Bones
3.4.1. Skin and Soft Tissue infections
3.4.1.1. Vesicles, Bullae, Crusted lesions, Folliculitis, Papular and Nodular Lesions,Ulcers with or without eschars, Erysipelas
3.4.1.2. Cellulitis
3.4.1.3. Necrotizing Fasciitis
3.4.1.4. Myositis/Myonecrosis
3.4.1.5. Infectious Arthritis
3.4.1.6. Osteomyelitis
3.5. Pneumococcal Infections
3.5.1. Pneumonia
3.5.2. Meningitis
3.5.3. Bacteremia, septic arthritis,endocarditis, pericarditis, peritonitis
3.5.4. Noninvasive syndromes: Sinusitis and otitis media
3.6. Staphylococcal Infections
3.6.1. S.aureus Infections
3.6.2. Coagulase-Negative Staphylococci infections
3.7. Streptococcal/Enterococcal Infections, Diptheria, Corynebacteria Infections & Related Species
3.7.1. Streptococcal and Enterococcal infections
3.7.2. Group A Streptococcus (GAS)
3.7.2.1. Pharyngitis
3.7.2.2. Scarlet Fever
3.7.2.3. Skin and Soft tissue infections
3.7.2.4. Pneumonia and empyema
3.7.2.5. Bacteremia
3.7.2.6. Toxic Shock syndrome
3.7.3. Streptococci of Groups C and G
3.7.4. Group B Streptococcus
3.7.5. Nonenterococcal Group D Streptococci
3.7.6. Viridans Streptococci
3.7.7. Enterococcal Infections
3.7.8. Corynebacterium Diphtheriae
4. Cardiology
4.1. Physical Examination of the Heart
4.1.1. Carotid Artery Pulse: Pulsus parvus, Pulsus tardus, Bounding pulse, Pulsus bisferiens, Pulsus alterans, Pulsus paradoxus
4.1.2. Jugular Venous Pulsations (JVP): Large "a" wave, Large "v" wave, Steep "y" descent, Slow "y" descent
4.1.3. Precordial Palpation: Forceful apical thrust, Lateral and downward displacement of apex impulse, Prominent presystolic impulse, Double systolic apical impulse. Sustained "lift"at lower left sternal border, Dyskinetic impulse
4.1.4. Auscultation
4.1.4.1. Heart Sounds: S1, S2, S3, S4, Opening snap, Ejection Clicks, Midsystolic clicks
4.1.4.2. Heart Murmurs
4.1.4.2.1. Systolic Murmurs: Ejection-type, Holosystolic, Late-systolic
4.1.4.2.2. Diastolic Murmurs: Early Diastolic, Mid-to-Late diastolic, Continous
4.2. Electrocardiography
4.2.1. Standard Approach to the ECG
4.2.1.1. Heart Rate,Rhythm, Mean axis
4.2.2. Intervals
4.2.2.1. PR interval (0.12-0.20sec)
4.2.2.2. QRS interval (0.06-0.10sec)
4.2.2.3. QT (<50% of RR interval; corrected QT <0.44s)
4.2.3. Hypertrophy
4.2.3.1. Infarction
4.2.4. ST-T waves
4.2.4.1. ST elevation
4.2.4.2. ST depression
4.2.4.3. Tall peaked T
4.2.4.4. Inverted T
4.3. Congenital Heart Disease in the Adult
4.3.1. Atrial Septal Defect (ASD)
4.3.1.1. PE:Prominent right ventricular impulse, wide fixed splitting of S2, systolic murmur from flow across pulmonic valve, diastolic flow rumble across tricuspid valve, prominent jugular venous v WAVE
4.3.1.2. ECG: Incomplete RBBB (rSR' in Right precordial leads)
4.3.1.3. Tx: Surgical or Percutaneous transcatheter closure, Antiarrythmic therapy
4.3.2. Ventricular Septal Defect (VSD)
4.3.2.1. PE: Systolic thrill and holosystolic murmur at lower sternal border, loud P2, S3, diastolic flow murmur across mitral valve
4.3.2.2. Tx; Diuretics and afterload reduction, Surgery closure
4.3.3. Patent Ductus Arteriosus
4.3.3.1. PE: Hyperactive LV impulse, loud continuous "machinery" murmur at upper left sternal border
4.3.3.2. Tx: if (-) pulmonary hypertension, PDA should be surgically ligated or divided to prevent infective endocarditis, LV dysfunction and pulmonary hypertension
4.3.4. Progression to Pulmonary Hypertension
4.3.4.1. PE: Loud P2, murmur of pulmonary valve regurgitation and signs of RV failure
4.3.5. Acyanotic Congenital Heart Lesions without a shunt
4.3.5.1. Pulmonic Stenosis
4.3.5.1.1. PE: RV hypertrophy and systolic "doming" of the pulmonic valve
4.3.5.1.2. Tx: Symptomatic or severe stenosis requires baloon valvuloplasty or surgical correction
4.3.5.2. Congenital Bicuspid Aortic Valve
4.3.5.2.1. PE: presence of a systolic ejection click
4.3.5.3. Coarctation of Aorta
4.3.5.3.1. PE: LV hypertrophy
4.3.5.3.2. Tx: Surgical correction
4.3.6. Complex Congenital Heart Lesions
4.3.6.1. Tetralogy of Fallot
4.3.6.1.1. PE: cyanosis and systemic hypoxemia
4.3.6.1.2. ECG: Right Ventricular hypertrophy
4.3.6.1.3. CXR: "boot-shaped" heart with prominent RV
4.3.6.2. Transposition of the Great Arteries
4.3.6.2.1. Echocardiography: aberrant anatomy
4.3.6.3. Eibstein Anomaly
4.3.6.3.1. Echocardiography: displacement of tricuspid septal leaflet, abnormal RV size, tricuspid regurgitation
4.3.7. Endocarditis Prophylaxis in Congenital Heart Disease
4.3.7.1. 1. Unrepaired cyanotic congenital heart disease
4.3.7.2. 2. Repaired congenital heart disease with residual defects adjacent to site of a prosthetic patch or transcatheter device
4.3.7.3. 3.A history of complete repair of congenital defects with prosthetic material or a transcatheter device within the previous 6 months
4.4. Valvular Heart Disease
4.4.1. Mitral Stenosis
4.4.2. Mitral Regurgitation
4.4.3. Mitral Valve Prolapse
4.4.4. Aortic Stenosis
4.4.5. Aortic Regurgitation
4.4.6. Tricuspid Stenosis
4.4.7. Tricuspid Regurgitation
4.5. Cardiomyopathies and Myocarditis
4.5.1. Dilated Cardiomyopathy (CMP)
4.5.2. Restrictive Cardiomyopathy
4.5.3. Hypertrophic Cardiomyopathy
4.5.4. Myocarditis
4.6. Hypertension
4.6.1. Systolic >140mmhg or diastolic >90mmhg
4.6.2. Secondary Hypertension due to:
4.6.2.1. Renal Artery Stenosis (Renovascular Hypertension)
4.6.2.2. Renal Parenchymal disease
4.6.2.3. Coarctation of Aorta
4.6.2.4. Pheochromocytoma
4.6.2.5. Hyperaldosteronism
4.6.3. Lab Work up:
4.6.3.1. Serum creatinine, BUN, Urinalysis
4.6.3.2. Serum K measured off diuretics
4.6.3.3. CXR
4.6.3.4. ECG
4.6.3.5. Blood tests including CBC, glucose, lipid levels, calcium, uric acid
4.6.3.6. Thyroid stimulating hormone
4.6.4. Tx: Control hypertension with minimal side effects. Diuretics, ACE inhibitors, Angiotensin II Receptor Blockers, Calcium antagonists, Beta blockers
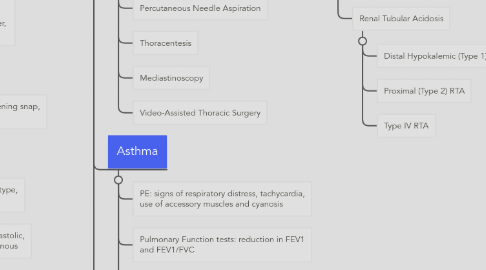
5. Pulmonology
5.1. Pulmonary Diagnostic Procedures
5.1.1. Radiographic Studies: Chest Xray
5.1.2. Nuclear Medicine Imaging
5.1.3. Sputum Exam
5.1.4. Bronchoscopy
5.1.5. Percutaneous Needle Aspiration
5.1.6. Thoracentesis
5.1.7. Mediastinoscopy
5.1.8. Video-Assisted Thoracic Surgery
5.2. Asthma
5.2.1. PE: signs of respiratory distress, tachycardia, use of accessory muscles and cyanosis
5.2.2. Pulmonary Function tests: reduction in FEV1 and FEV1/FVC
5.2.3. Blood tests:CBC may show eosinophilia, total serum IgE is markedly elevated in allergic bronchopulmonary aspergillosis, s
5.2.4. Chest Xray usually normal
5.2.5. Tx: Bronchodilators, ICS, limiting exposure to environmental triggers
5.3. Chronic Obstructive Pulmonary Disease
5.3.1. airflow obstruction determined by a reduced ratio of the forced expiratory voulume in 1s to the forced vital capacity
5.3.2. Gold Criteria for COPD severity: 0-At risk, I-Mild,IIA-Moderate,III-Severe, IV-Very severe
5.3.3. History: have smoked >20pack-years of cigarettes, cough and phlegm production, with chronic productive cough for 3 months per year
5.3.4. PE: may be normal, signs of hyperinflation may become more prominent (barrel chest and poor diaphragmatic excursion), COPD exacerbations (signs of respiratory distress, tachycardia, tachypnea, use of accessory muscles of respiration and cyanosis
5.3.5. Chest Xray may show hyperinflation, emphysema and pulmonary hypertension
5.3.6. Pulmonary Function test: FEV1/FVC ratio is reduced below 0.7
5.3.7. Lab test: a1 antitrypsin, arterial blood gases, CBC
5.3.8. Tx: Smoking cessation, Pulmonary rehabilatation, bronchodilators, corticosteroids, oxygen, lung volume reduction surgery and lung transplantation for end-stage COPD
6. Renal Tubular Disease
6.1. caused by Toxins, neoplasia, immune disorders, vascular disorders, hereditary renal diseases, infecious injury
6.2. Acute Interstitial Nephritis
6.3. Chronic Interstitial Nephritis
6.4. Monoclonal Immunoglobulins and Renal disease
6.5. Polycystic kidney disease
6.6. Renal Tubular Acidosis
6.6.1. Distal Hypokalemic (Type 1) RTA
6.6.2. Proximal (Type 2) RTA
6.6.3. Type IV RTA
7. Nephrology
7.1. Patient with Renal Dse.
7.1.1. Acute Renal Injury
7.1.2. rapid, severe decrease in glomerular infiltration rate (rise in serum creatinine and BUN), with reduced urine output
7.1.3. Rapidly Progressive Glomerulonephritis
7.1.4. Acute Glomerulonephritis
7.1.5. Chronic Renal Failure
7.1.6. Nephrotic Syndrome
7.1.7. Asymptomatic Urinary abnormalities
7.1.8. Urinary tract infection
7.1.9. Renal Tubular defects
7.1.10. Hypertension
7.2. Acute Renal Failure
7.2.1. increase in serum creatinine concentration usually increase of 50% or absolute increase by 44-88umol/L
7.2.2. Prerenal, Intrinsic, Postrenal
7.2.3. AKI manifests azotemia, orthostatic hypotension, tachycardia, low jugular venous pressure, and dry mucous, jugular venous distention, S3 gallop, and peripheral edema
7.2.4. Tx:Supportive care, high dose glucocorticoids, cytotoxic agents, plasmapheresis, plasma exchange, antibiotic therapy,dialysis
7.3. Chronic Kidney Disease
7.3.1. long standing, irreversible impairment of kidney function
7.3.2. Tx:Control of hypertension, ACE inhibitors and ARBs, diuretics
7.4. Glomerular Diseases
7.4.1. Acute glomerulonephritis
7.4.1.1. Acute Poststreptococcal GN
7.4.1.2. Postinfectious GN
7.4.2. Rapidly Progressive Glomerulonephritis
7.4.2.1. SLE (lupus)
7.4.2.2. Antineutrophil Cytoplasmic Antibody (ANCA)-associated, Pauci-immune GN
7.4.2.3. Anti-glomerular basement membrane disease
7.4.2.4. Henoch-Schonlein Purpura
7.4.3. Nephrotic Syndrome
7.4.3.1. Minimal Change Disease
7.4.3.2. Membranous GN
7.4.3.3. Focal Glomerulosclerosis (FGS)
7.4.3.4. Membranoproliferative Glomerulonephritis (MPGN)
7.4.3.5. Diabetic Nephropathy
7.4.4. Asymptomatic Urinary abnormalities
7.4.4.1. Thin basement membrane nephropathy
7.4.4.2. IgA Nephropathy
7.4.4.3. Glomerulopathies associated with Multisystem dse
8. Gastroenterology
8.1. Peptic Ulcer Disease
8.1.1. H.pylori, NSAIDs, Zollinger,Ellison syndrome
8.1.2. Duodenal ulcer
8.1.2.1. burning epigastric pain 90 min to 3 h after meals, nocturnal and relieved by food
8.1.3. Gastic Ulcer
8.1.3.1. burning epigastric pain made worse by or unrelated to food, anorexia, food aversion, weight loss
8.1.4. diagnosed by Upper endoscopy or upper GI barium radiography
8.1.5. detection of H.pylori: (+) antibodies in serum, rapid urease test of antral biopsy, urea breath test to confirm eradication of H.pylori, fecal antigen test
8.1.6. Tx: discontinue NSAIDs, smoking cessation, H2 receptor blockers, sucralfate, antacids, PPis, Surgery for complications
8.2. Acute Hepatitis
8.2.1. Acute Viral hepatitis
8.2.1.1. malaise, nausea & vomiting, diarrhea, low grade fever ff. by dark urine, jaundice, & tender hepatomegaly, elevated AST & ALT
8.2.1.2. Hepatitis A (fecal-oral)
8.2.1.2.1. Dx: IgM anti-HAV in acute or early convalescent serum sample
8.2.1.2.2. Prevention: After exposure ( immune globulin 0.02mL/kg IM within 2 weeks) Before exposure (inactivated HAV vaccine 1mL IM)
8.2.1.3. Hepatitis B (percutaneous, sexual or perinatal transmission)
8.2.1.3.1. Dx: HBsAg in serum, IgM anti-HBc, HBV DNA in serum
8.2.1.3.2. Prevention: After exposure in unvaccinated persons: HBIg 0.06mL/kg IM within 14days of sexual exposure, HBIg 0.05mL in thigh after birth started within first 12h of life for perinatal exposure
8.2.1.4. Hepatitis C (IV drug use, transfusion associated
8.2.1.4.1. Dx: Anti-HCV in serum, HCV RNA
8.2.1.4.2. Prevention: testing of donated blood for anti HCV,
8.2.1.5. Hepatitis D (HbsAg+IV drug users or by transfusion in hemophiliacs, HbsAg+men who have sex with men
8.2.1.5.1. Dx: Anti-HDV in serum
8.2.1.5.2. Prevention: Hepatitis B vaccine for noncarriers only
8.2.2. Tx: Activity as tolerated, high-calorie diet, IV hydration, cholestyramine 4g PO for pruritus, liver transplantation for fulminant hepatic failure and grades III-IV encephalopathy
8.3. Chronic Hepatitis
8.3.1. chronic inflammatory reaction in the liver for atleast 6 months
8.3.2. HBV,HCV, HDV, drugs (methyldopa, nitrofurantoin, isoniazid, dantrolene)
8.3.3. classified by grade and stage, assessment of necrosis and inflammatory activity and examination of liver biopsy
8.3.4. fatigue,malaise, anorexia, low grade fever, jaundice, complications of cirrhosis (ascites, variceal bleeding, hypersplenism)
8.3.5. Tx: IFN-a, PEG IFN, lamivudine, adefovir dipivoxil, telbivudine, and tenofovir
9. Rheumatology
9.1. Systemic Lupus Erythematosus (SLE)
9.1.1. tissues and cells undergo damage mediated by tissue-binding autoantibodies and immune complexes
9.1.1.1. fatigue,fever,malaise, weight loss, malar "butterfly" rash, photosensivity, vasculitis, alopecia, oral ulcers, arthritis, anemia, neutropenia, thrombocytopenia, lymphadenopathy, pleuritis, pericarditis
9.1.1.2. presence of ANA (not specific), antibodies to dsDNA, ssDNA, Sm, Ro, LA, histone, Complement levels (C3, C4, CH50), serum immunoglobulins, VDRL, PT, PTT, anticardiolipin, lupus anticoagulant, urinalysis
9.1.2. Tx: NSAIDs, antimalarials, Belimumab (Non-Life-Threatening SLE), systemic glucocorticoids, cytotoxic/ immunosuppressive agents like Cyclophosphamide, Mycophenolate mofetil, Azathioprine ( Life-Threaning SLE)
9.2. Systemic Sclerosis
9.2.1. thickening of skin, involvement of multiple organs
9.2.2. Cutaneous (edema, fibrosis, telangiectasis, calcinosis, Raynaud's phenomenon), Arthralgias an arthritis, GI ( esophageal hypomotility, intestinal hypofunction, Pulmonary (fibrosis, pulmonary hypertension, alveolitis), Cardiac ( pericarditis, cardiomyopathy), Renal (hypertension, renal crisis)
9.2.3. Lab: ESR, ANA, Antitopoisomerase I, UA
9.2.4. Radiographs: CXR, barium swallow, hand xrays, ECG, echo
9.2.5. Tx: Warm clothing, smoking cessation, Calcium channel blockers, ACE inhibitors, Antacids, PPIs, D-Penicillamine, Glucocorticoids, Cyclophosphamide, Epoprostenol and Bosentan
9.3. Vasculitis
9.3.1. inflammation and damage to blood vessels, compromising vessel lumen, resulting to ischemia
9.3.2. Primary Vasculitis Syndromes
9.3.2.1. Granulomatosis with Polyangiitis (Wegener's)
9.3.2.2. Churg-Strauss syndrome
9.3.2.3. Polyarteritis Nodosa (PAN)
9.3.2.4. Microscopic Polyangiitis
9.3.2.5. Giant Cell arteritis
9.3.2.6. Takayasu's Arteritis
9.3.2.7. Henoch-Schonlein Purpura
9.3.3. Thorough History and Physical exam for ischemic manifestations and systemic inflammatory signs/symptoms
9.3.4. Lab: CBC, ESR, renal function tests, UA, ANA, rheumatoid factor, anti-GBM, hepatitis B/C serologies, HIV
9.3.5. ANCA for Wegener's granulomatosis, microscopic polyangiitis, Churg-Strauss syndrome
9.3.6. CXR performed even in the absence of symptoms
9.3.7. Dx: Arteriogram or biopsy of affected organs
10. Endocrinology and Metabolism
10.1. Diabetes Mellitus
10.1.1. Type 1 DM
10.1.1.1. insulin deficiency, tendency to develop to ketosis
10.1.2. Type 2 DM
10.1.2.1. insulin resistance, impaired insulin secretion, excessive hepatic glucose production
10.1.3. Dx: Fasting plasma glucose >7.0mmol/L or >126mg/dL, 2h plasma glucose >11.1mmol/L or >200mg/dL during a 75g oral glucose tolerance test, Hemoglobin A1c >6.5%
10.1.4. polyuria,polydipsia,weight loss, fatigue, weakness, blurred vision, poor wound healing
10.1.5. Tx: education about nutrition, exercise, medications to lower the plasma glucose,
10.1.5.1. for Type 1 DM 0.5-1.0 U/kg per day of insulin into multiple doses (injection of glargine at bedtime with preprandial lispro, glulisine or insulin aspart or continuous SC insulin using infusion device
10.1.5.2. for Type 2 DM, maged with diet and exercise alone or in conjunction with oral glucose-loweing agents, insulin or oral agents + insulin, GLP-1 (exenatide and liraglutide) + metformin/sulfonylureas

