1. Terminology
1.1. Action Spectrum
1.2. Absorption Spectrum
1.3. MED
1.3.1. The unit of measurement of sunburn
1.3.2. The minimum UVL exposure that produces a clearly marginated erythema in the irradiated site 24 hours after a single exposure
1.3.3. Units
1.3.3.1. UVA
1.3.3.1.1. J/cm2
1.3.3.2. UVB
1.3.3.2.1. mJ/cm2
1.4. SPF
1.4.1. Amount of UVB* Energy (Protected/Unprotected)
1.4.2. There is a popular misconception that SPF relates to time of solar exposure.
1.5. Photo-Toxic Reaction
1.5.1. Exaggerated reaction to UVR-induced activation of a phototoxic agent (i.e., Exacerbated Sunburn)
1.5.2. Non-immunologic Phenomenon
1.5.2.1. Reproducible in every individual
1.5.2.2. No prior sensitization required
1.6. Photo-Allergic Reaction
1.6.1. DTH (Type IV hypersensitivity reaction)
1.6.2. Only previously sensitized individuals develop a photo-allergy
1.6.3. Most Common Causes
1.6.3.1. Sunscreens (US)
1.6.3.1.1. Especially benzophenone-3 (oxybenzone)
1.6.3.2. NSAIDs (Germany, Austria and Switzerland)
1.7. Photo-sparing areas of the Head and Neck
1.7.1. Wilkinson’s triangle (behind the ears)
1.7.2. Nasolabial folds
1.7.3. Submandibular Neck
1.7.4. Contact dermatitis involves these areas
1.8. Units
1.8.1. Watt
1.8.2. Joule
1.9. UV Hardening
2. General
2.1. Skin Phototypes
2.1.1. I
2.1.1.1. Always Burns, Never Tans
2.1.2. II
2.1.2.1. Usually Burns, Tans with Difficulty
2.1.3. III
2.1.3.1. Sometimes Mild Burn, Gradually Tans
2.1.4. IV
2.1.4.1. Rarely Burns, Tans with Ease
2.1.5. V
2.1.5.1. Very Rarely Burns, Tans Very Easily
2.1.6. VI
2.1.6.1. Never Burns, Tans Very Easily
2.2. Wavelengths (nm)
2.2.1. Infrared
2.2.2. Visible (400-750)
2.2.2.1. ROY-G-BV
2.2.2.1.1. Violet (400-450)
2.2.2.1.2. Blue (450-495)
2.2.2.1.3. Green (495-570)
2.2.2.1.4. Yellow (570-590)
2.2.2.1.5. Orange (590-620)
2.2.2.1.6. Red (620-750)
2.2.3. UVA (320-400)
2.2.3.1. UVA 1 (340-400)
2.2.3.2. UVA 2 (320-340)
2.2.3.3. Wood's Light (365)
2.2.4. UVB (290-320)
2.2.4.1. Narrowband UVB (311-312)
2.2.4.2. Excimer Laser (308)
2.2.4.3. 290 nm (Peak Melanogenesis)
2.2.4.4. 300 nm (Most Erythemogenic)
2.2.4.5. 352 nm (Photo-testing and PUVA Peak Emission)
2.2.5. UVC (200-290)
2.2.5.1. UV Light Source
2.2.5.1.1. Mercury Vapor Lamps (254)
2.3. Depth of photon skin penetration is directly proportional to wavelength
2.3.1. UVB
2.3.1.1. 2-5% UVB reaches the skin
2.3.1.2. Out of this, only 14% reaches melanocytes and lower epidermis
2.3.2. UVA
2.3.2.1. Less affected by environment (penetrates: Clouds and Glass)
2.3.2.2. Up to 50% reach the depth of melanocytes and the dermal compartment
2.3.2.3. The total photon energy delivered into the lower epidermis and upper dermis (100 UVA > UVB)
2.4. UVA
2.4.1. UVA Facts
2.4.1.1. Causes photoallergic and phototoxic contact dermatitis
2.4.1.2. Photo-patch testing is done with UVA
2.4.1.2.1. If UVA-sensitive patient?
2.4.1.3. see Photocancerogenesis
2.4.1.4. See Action Spectra
2.4.2. UVA Therapies
2.4.2.1. PUVA
2.4.2.1.1. Cancerogenicity
2.4.2.1.2. Safe for HIV-infected psoriasis patients
2.4.2.2. Tar Smarts
2.4.3. Photopheresis
2.4.3.1. PO 8-MOP --> venous blood draw --> Photopheresis machine separates and exposes mononuclear cells (buffy coat) to 2 J/cm2 of UVA --> re-infusion
2.4.3.2. Induction of an immune response to malignant cells is postulated
2.4.3.3. Works better if
2.4.3.3.1. (CD4/CD8) < 10
2.4.3.3.2. Normal LDH
2.4.3.3.3. Indications
2.5. UVB
2.5.1. UVB Facts
2.5.1.1. SPF is measured based on UVB
2.5.1.2. UVB erythema reaches a maximum in 6 to 24 hours
2.5.1.3. Most effective for?
2.5.1.3.1. Suppressing cutaneous immunity
2.5.1.3.2. UVL treatment modality for?
2.5.1.3.3. Inducing neoplasia in mice
2.5.2. UVB Therapies
2.5.2.1. Excimer Laser (308 nm)
2.5.2.2. Narrowband UVB (311-312 nm)
2.5.2.2.1. The peak of NB-UVB spectrum = 10x the peak of BB-UVB curve
2.5.2.2.2. Significantly less erythemogenic (therefore less cancerogenic) than BB-UVB
2.5.2.2.3. Thus, more therapeutic UVB can be delivered before sunburn
2.5.2.2.4. No association between NB-UVB and NMSC
2.5.2.3. Side Effects
2.5.2.3.1. Broad Band
2.5.2.3.2. Treatment
2.5.2.3.3. Narrowband
2.6. UVC
2.6.1. Arc Welders
2.7. Action Spectra
2.7.1. by Condition
2.7.1.1. PMLE
2.7.1.1.1. UVA
2.7.1.2. Drug-Induced Photosensitivity
2.7.1.2.1. UVA and/or UVB
2.7.1.3. CAD
2.7.1.3.1. UVB
2.7.1.4. Solar Urticaria
2.7.1.4.1. Visible Light
2.7.1.5. Photo-Contact Dermatitis
2.7.1.5.1. UVA
2.7.1.6. Hydroa Vacciniforme
2.7.1.6.1. UVA
2.7.1.7. Lupus Erythematosus
2.7.1.7.1. UVB
2.7.1.8. Xeroderma Pigmentosum
2.7.1.8.1. UVB
2.7.2. by UV Type
2.7.2.1. UVA
2.7.2.1.1. PMLE
2.7.2.1.2. Hydroa Vacciniforme
2.7.2.1.3. Photo-Contact Dermatitis
2.7.2.1.4. Drug-Induced Photosensitivity
2.7.2.2. UVB
2.7.2.2.1. CAD
2.7.2.2.2. Lupus Erythematosus
2.7.2.2.3. Xeroderma Pigmentosum
2.7.2.3. Visible Light
2.7.2.3.1. Solar Urticaria
2.8. Sunscreens
2.8.1. SPF measures UVB coverage
2.8.1.1. SPF+ denotes UVA coverage
2.8.1.2. FDA uses 2 mg/cm2 of sunscreen in testing
2.8.2. The best UVA protection is provided by products that contain zinc oxide, avobenzone, and ecamsule
2.8.2.1. Titanium dioxide does not cover UVA spectrum completely
2.8.3. The best protection is achieved by application 15–30 minutes before exposure, followed by one reapplication 15–30 minutes after the sun exposure begins. Further reapplication is only necessary after activities such as swimming, sweating, or rubbing/wiping.
2.8.4. People commonly apply only 1/2 to 1/4 of the amount recommended
2.8.5. One study indicates that the relation between SPF and sunscreen quantity follows exponential growth. Application of 1 mg cm−2 or 0·5 mg cm−2 makes the SPF fall as the square or fourth root, respectively, and 4 mg cm−2 results in an almost squared SPF. (Br. J. Dermatol., 156: 716–719.)
2.9. Phototesting
2.9.1. Used for the patients suspected of photosensitivity
2.9.2. Done on the unaffected and untanned skin of the gluteal area, lower back or ventral forearms.
2.9.3. 6 test squares of increasing UV doses
2.9.4. MED
2.9.4.1. The dose of UVR that produces minimal erythema that completely fills the test square
2.9.4.2. Read 24 hours after exposure
2.9.5. Only the patients with possible solar urticaria are evaluated until 30 minutes after exposure
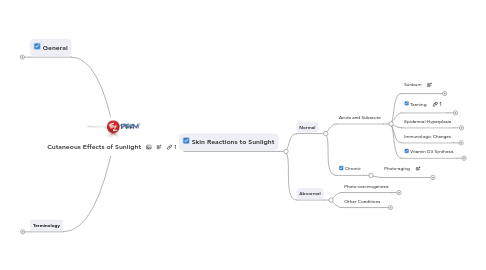
3. Skin Reactions to Sunlight
3.1. Normal
3.1.1. Acute and Subacute
3.1.1.1. Sunburn
3.1.1.1.1. Erythemogenicity: UVB = 1000 UVA
3.1.1.1.2. Wavelengths
3.1.1.2. Tanning
3.1.1.2.1. Immediate/Persistent Pigment Darkening
3.1.1.2.2. Delayed Tanning (DT):
3.1.1.3. Epidermal Hyperplasia
3.1.1.3.1. Due to UVB and UVC, but generally not UVA exposure
3.1.1.3.2. It adds to UVR protection
3.1.1.3.3. Histologically evident within days and persists for weeks
3.1.1.4. Immunologic Changes
3.1.1.4.1. Photo-Immunosuppression
3.1.1.4.2. UVB>UVC>>>UVA
3.1.1.5. Vitamin D3 Synthesis
3.1.1.5.1. Hormone (not a vitamin)
3.1.1.5.2. Synthesis
3.1.1.5.3. 25(OH)D
3.1.1.5.4. Protects against the development of many chronic diseases and cancer
3.1.1.5.5. Types
3.1.1.5.6. Only vitamin D + Calcium leads to decreased risk of hip fractures, and not vitamin D alone
3.1.1.5.7. Adequate Daily Intake is very controversial
3.1.2. Chronic
3.1.2.1. Photo-aging
3.1.2.1.1. Important role of UVA
3.1.2.1.2. Conditions
3.2. Abnormal
3.2.1. Photo-carcinogenesis
3.2.1.1. Molecular Genetics
3.2.1.1.1. DNA Damage
3.2.1.1.2. Nucleotide Excision Repair
3.2.1.1.3. Tumor Supressor Genes
3.2.1.1.4. Proto-Oncogene
3.2.1.1.5. Oncogene
3.2.1.2. Nevoid Basal Cell Carcinoma
3.2.1.2.1. Inheritance
3.2.1.2.2. Defect
3.2.1.2.3. Pathogenesis
3.2.1.3. Melanoma and UVA Controversy
3.2.1.3.1. Epidemiological Observations
3.2.1.3.2. Laboratory Observations
3.2.1.4. UVA
3.2.1.4.1. PUVA
3.2.1.4.2. UVA does not cause melanoma in fish model
3.2.1.5. UVB
3.2.1.5.1. UVB is the action spectrum for Melanoma development (the best supported evidence)
3.2.1.6. Life-Style
3.2.1.6.1. Intermittent UVR Exposure
3.2.1.6.2. Chronic Exposure (Life Time UV Exposure Dose)
3.2.1.6.3. Tanning Beds
3.2.1.7. Body Locations
3.2.1.7.1. Melanoma: more common on the Trunk in Men, and Lower Extremities in Women
3.2.2. Other Conditions
3.2.2.1. Idiopathic (Immunologic)
3.2.2.2. Phototoxicity and Photoallergy
3.2.2.2.1. (Sunburn)
3.2.2.2.2. Photosensitizing Medications
3.2.2.2.3. Photosensitizing Topical Agents
3.2.2.2.4. Chemical-Induced
3.2.2.2.5. Phytophotodermatitis
3.2.2.3. Photo-Aggravated Dermatoses
3.2.2.3.1. Acne vulgaris
3.2.2.3.2. Atopic dermatitis
3.2.2.3.3. Bullous pemphigoid
3.2.2.3.4. Carcinoid syndrome
3.2.2.3.5. Cutaneous T-cell lymphoma
3.2.2.3.6. Dermatomyositis
3.2.2.3.7. Disseminated superficial actinic porokeratosis (DSAP)
3.2.2.3.8. EM
3.2.2.3.9. Familial benign chronic pemphigus (Hailey–Hailey disease)
3.2.2.3.10. Hartnup syndrome
3.2.2.3.11. Keratosis follicularis (Darier disease)
3.2.2.3.12. Lichen planus
3.2.2.3.13. Lupus erythematosus
3.2.2.3.14. Pellagra
3.2.2.3.15. Pemphigus, including pemphigus foliaceus (erythematosus)
3.2.2.3.16. PRP
3.2.2.3.17. Psoriasis
3.2.2.3.18. Reticular erythematous mucinosis (REM)
3.2.2.3.19. Rosacea
3.2.2.3.20. Seborrheic dermatitis
3.2.2.3.21. Transient acantholytic dermatosis (Grover's disease)
3.2.2.3.22. Viral infections (including herpes simplex)
3.2.2.4. Metabolic
3.2.2.4.1. see Porphyrias
3.2.2.5. Nutritional
3.2.2.5.1. Pellagra
3.2.2.6. Genodermatoses
3.2.2.7. Phytophoto-Allergic Contact Dermatitis
3.2.2.7.1. A phototoallergic reaction have been described to ?
