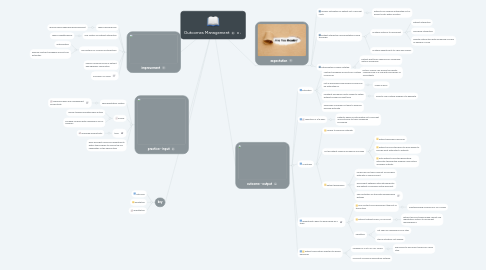
1. improvement
1.1. reduce billing errors
1.1.1. reduce failed medicare reimbursement
1.2. one system for patient interaction
1.2.1. reduce repetitiveness
1.3. one system for insurance interactions
1.3.1. authorization
1.3.2. defined contract allowable amounts for estimates
1.4. reduce common errors in patient demographic information
1.5. increase CMI value
2. practice - input
2.1. new registration system
2.1.1. improved labor and management productivity
2.2. money
2.2.1. money toward operating new system
2.2.2. increase revenue with meaningful use of program
2.3. time
2.3.1. improved productivity
2.4. work amongst numerous departments within the program to ensure the full capabilities of the new system
3. key
3.1. outcome
3.2. qualitative
3.3. quantitative
4. expectation
4.1. quicker estimates for patient out of pocket costs
4.1.1. patients can receive anticipated out of pocket costs within minutes
4.2. patient interaction documentations more thorough
4.2.1. multiple systems to document
4.2.1.1. patient interaction
4.2.1.2. insurance interaction
4.2.1.3. hospital interaction with increasing success of delivery of care
4.2.2. multiple departments to view discussions
4.3. authorizations clearly notated
4.3.1. patient wait times reduced for scheduled date of procedure
4.3.2. doctor's offices can ensure the facility rendering care is in line with insurances of their patients
5. outcome - output
5.1. estimates
5.1.1. contract allowable amounts for multiple insurances
5.1.2. not all procedures physicians provide can be estimated for
5.1.2.1. reads as error
5.1.3. inpatient procedure costs unable to obtain without proper account type
5.1.3.1. need to use multiple programs to generate
5.1.4. secondary coverage not able to produce possible estimate
5.2. reduction in A/R days
5.2.1. patients aware of anticipated out-of-pocket amounts prior to their scheduled procedure
5.3. IT glitches
5.3.1. unable to produce estimate
5.3.2. not all patient medical insurances included
5.3.2.1. patient experience declines
5.3.2.2. patient access staff have to work harder to provide best estimates to patients
5.3.2.3. both patients and staff generating estimates through the program lose faith in unreliable outputs
5.3.3. patient experience
5.3.3.1. receive bill for twice amount of provided estimate or same amount
5.3.3.2. disconnect between estimate generator and patient's insurance actual payment
5.3.3.3. see frustration of staff with unaddressed glitches
5.4. departments have to work harder as a team
5.4.1. one contact could disconnect the rest of the system
5.4.1.1. inputing wrong insurance or CPT codes
5.4.2. without patient orders, no account
5.4.2.1. without account being made cannot use registration system to document demographics
5.4.3. repetition
5.4.3.1. not seen as meaningful by all staff
5.4.3.2. staff motivation not aligned
5.5. patient information directed to wrong personnel
5.5.1. unaware of ICD10 or CPT codes
5.5.1.1. physicians to document codes for office staff
5.5.2. incorrect insurance information entered
