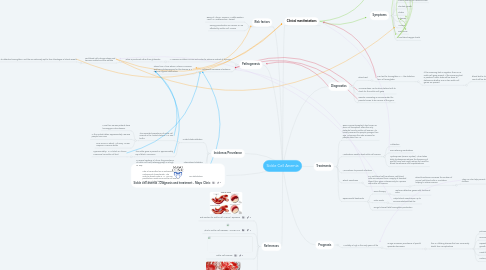
1. Sickle cell anemia - Diagnosis and treatment - Mayo Clinic
2. Risk factors
2.1. Being of African, Hispanic, Middle Eastern, Asian, or Mediterranean decent
2.2. Having parents who are carriers, or are affected by Sickle Cell Anemia
3. Pathogenesis
3.1. A missense mutation occurs and codes for adenine instead of thymine.
3.1.1. Valine is produced rather than glutamate
3.1.1.1. Red blood cells change shape and become sickled and less soluble
3.1.1.1.1. Sickled rbc can carry less O2 due to defective hemoglobin, and the are extremely apt to form blockages in blood vessels
3.2. Autosomal Recessive Inheritance
3.2.1. Stems from Africa where Malaria is common and being heterozygous for this disease is a defense against contraction
4. References
4.1. Risk Factors for Sickle Cell Anemia | TapGenes
4.2. What Is Sickle Cell Disease? - NHLBI, NIH
4.3. Sickle Cell Disease
4.4. Sickle Cell Anemia | Sickle Cell Disease | MedlinePlus
5. Incidence/Prevelance
5.1. United States statistics
5.1.1. The expected prevalence of sickle cell anemia in the United States is 1 in 625 births
5.1.1.1. More than 30,000 patients have homozygous HbS disease.
5.1.1.2. In the United States, approximately 100,000 people have SCD
5.1.1.3. SCD occurs in about 1 of every 16,300 Hispanic-American births
5.1.2. The sickle gene is present in approximately 8% of black Americans
5.1.2.1. Approximately 1 in 13 black or African Americans has sickle cell trait
5.2. International statistics
5.2.1. In several sections of Africa, the prevalence of sickle cell trait (heterozygosity) is as high as 30%
5.3. Sex distribution
5.3.1. HbS is transmitted as an autosomal codominant characteristic. The male-to-female ratio is 1:1. No sex predilection exists, since sickle cell anemia is not an X-linked disease
6. Symptoms
6.1. Yellow eyes
6.2. Painful swelling of hands and feet
6.3. Stunted growth
6.4. Stroke
6.5. Paleness
6.6. Anemia
6.7. Dark urine
6.8. Low blood oxygen levels
7. Signs
7.1. Pain episodes
7.2. Dizziness
7.3. Fatigue
8. Treatments
8.1. Bone marrow transplant, also known as stem cell transplant, offers the only potential cure for sickle cell anemia. It's usually reserved for people younger than age 16 because the risks increase for people older than 16.
8.2. Medications used to treat sickle cell anemia
8.2.1. Antibiotics
8.2.2. Pain-relieving medications
8.2.3. Hydroxyurea (Droxia, Hydrea). When taken daily, hydroxyurea reduces the frequency of painful crises and might reduce the need for blood transfusions and hospitalizations
8.3. Vaccinations to prevent infections
8.4. Blood Transfusion
8.4.1. In a red blood cell transfusion, red blood cells are removed from a supply of donated blood, then given intravenously to a person with sickle cell anemia.
8.4.1.1. Blood transfusions increase the number of normal red blood cells in circulation, helping to relieve anemia
8.4.1.1.1. They can also help prevent strokes in young children
8.5. Experimental treatments
8.5.1. Gene therapy
8.5.1.1. replaces defective genes with functional ones
8.5.2. Nitric oxide
8.5.2.1. Helps blood vessels open up to accommodate sickled rbc
8.5.3. Drugs to boost fetal hemoglobin production
9. Clinical manifestations
10. Diagnostics
10.1. Blood Test
10.1.1. Can test for hemoglobin S — the defective form of hemoglobin
10.1.1.1. If the screening test is negative, there is no sickle cell gene present. If the screening test is positive, further tests will be done to determine whether one or two sickle cell genes are present.
10.1.1.1.1. blood test to check for a low red blood cell count will be done.
10.2. Amniocentesis can be done before birth to check for the Sickle Cell gene
10.3. Genetic counseling is recommended for parents known to be carriers of the gene.
11. Prognosis
11.1. Mortality is high in the early years of life
11.1.1. as age increases, prevalence of painful episodes decreases
11.1.1.1. this is a lifelong disease that can cause early death from complications
11.1.1.1.1. pulmonary hypertension
11.1.1.1.2. economic loss and disability
11.1.1.1.3. Repeated infarction of joints, bones, and growth plates leads to aseptic necrosis
11.1.1.1.4. Hand-foot syndrome
11.1.1.1.5. Leukocytosis
