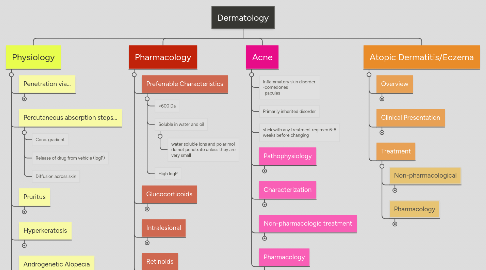
1. Physiology
1.1. Penetration via...
1.1.1. Intact stratum corneum
1.1.2. Sweat ducts
1.1.3. Sebaceous follicle
1.2. Percutaneous absorption steps...
1.2.1. Conc. gradient
1.2.2. Release of drug from vehicle (logP)
1.2.3. Diffusion across skin
1.3. Pruritus
1.3.1. dry skin, atopic eczema, urticaria, infestations
1.3.2. Caused By...
1.3.2.1. bites and parasites
1.3.2.2. dermatitis herpetiformis
1.3.2.3. atopic dermatitis
1.3.2.4. exfoliative dermatitis
1.3.2.5. jaundice
1.3.2.6. leukemia
1.3.2.7. hodgkins disease
1.3.3. Treated with...
1.3.3.1. emollients for xerosis
1.3.3.2. topical glucocorticoids
1.3.3.3. PO sedating antihistamines
1.3.3.4. ondansetron
1.3.3.5. UVB radiation
1.4. Hyperkeratosis
1.4.1. thickening of stratum corneum
1.4.1.1. calluses
1.4.1.2. verrucae (warts)
1.4.2. treat with...
1.4.2.1. keratolytic agents
1.4.2.1.1. lactic acid
1.4.2.1.2. salicylic acid
1.4.2.1.3. glycolic acid
1.4.2.1.4. urea
1.4.2.1.5. sulfur
1.4.2.2. destructive agents
1.4.2.2.1. pdophyllum resin for warts
1.5. Androgenetic Alopecia
1.5.1. most common cause of hair loss in adults 40+
1.5.2. dihydrosterone binds androgen receptors in follicles, and this activates the genes responsible for miniaturized vellus follicles
1.5.3. Treat with...
1.5.3.1. Minoxidil
1.5.3.1.1. originally a HTN drug
1.5.3.1.2. enhances follicle size
1.5.3.2. Finasteride
1.5.3.2.1. inhibits type II isozyme of 5 reductase (enzyme that converts testosterone to dihydrotestosterone
2. Acne
2.1. Inflammatory skin disorder -comedones -papules
2.2. Primarily inherited disorder
2.3. stick with any treatment regimen 6-8 weeks before changing
2.4. Pathophysiology
2.4.1. Contributing factors...
2.4.1.1. trauma
2.4.1.2. UV light
2.4.1.3. humid or hot conditions
2.4.1.4. emotions
2.4.1.5. corticosteroids, OCs, some antiepileptics
2.4.1.6. endocrine disorders
2.4.1.7. luteal phase of menstruation
2.4.2. Mechanism...
2.4.2.1. pilosebaceous units
2.4.2.2. production of androgens - cause sebaceous gland to enlarge
2.4.2.3. inflammatory acne caused by ruptured folicles
2.4.2.3.1. papule: solid red or brown elevation
2.4.2.3.2. pustule: papule filled with pus
2.4.2.3.3. nodule: severe acne, firm, warm, tender
2.4.2.3.4. cyst: inflamed, pus-filled nodule
2.4.2.4. hormonal acne
2.4.2.4.1. first line therapy...
2.4.2.4.2. Alt therapy
2.4.3. Plugged sebaceous follicles
2.4.3.1. open comedones = black heads (not dirt)
2.4.3.2. closed comedone = white head
2.5. Characterization
2.5.1. mild
2.5.1.1. comedones with or without pustules or papules
2.5.1.2. treat with
2.5.1.2.1. benzoyl peroxide
2.5.1.2.2. salicylic acid
2.5.1.2.3. topical retinoid
2.5.1.2.4. topical abx
2.5.2. moderate
2.5.2.1. comedones, several pustules or papules, with or without several nodules
2.5.2.2. treat with
2.5.2.2.1. topical retonoid + topical or PO abx
2.5.3. severe
2.5.3.1. extensive pustules or papules and many nodules, extensive scarring, drainage, formation of sinus tract
2.5.4. very severe
2.5.4.1. oral isotretinoin
2.6. Non-pharmacologic treatment
2.6.1. extraction
2.6.2. reduce triggers
2.6.3. hygeine
2.6.3.1. wash face no more than 2x/d
2.6.3.2. avoid antibacterial soaps
2.6.3.3. use soapless cleanser
2.6.4. moisturizer
2.6.4.1. oil fee
2.6.4.2. non-comedogenic
2.6.4.3. with sunscreen
2.7. Pharmacology
2.7.1. Antibiotics
2.7.1.1. topical
2.7.1.1.1. for superficial infections
2.7.1.1.2. must be used in combination with other products
2.7.1.1.3. Clindamycin
2.7.1.1.4. Erythromhcin
2.7.1.1.5. Tetracycline: use sunscreen
2.7.1.2. systemic
2.7.1.2.1. pt should never be on a PO abx as monotherapy. use for the shortest duration possible, and d/c after 3 months
2.7.1.2.2. possible OC failure
2.7.1.2.3. deeper infections
2.7.1.2.4. acne vulgaris
2.7.1.2.5. suppresses leukocyte chemotacxis
2.7.2. keratolytic: unclogs pores
2.7.3. comedolytic
2.7.3.1. topical retiniods
2.7.3.1.1. adapalene (Differin): less effective but less irritating
2.7.3.1.2. tarazotene (Tazorac): most effective and irritating
2.7.3.1.3. Tretinoin (Retin A): more effective than adapalene
2.7.4. PO retinoids
2.7.4.1. isotretinoin (Amnesteen, Accutane, Clavarris): severe inflammatory acne only
2.7.4.1.1. pregnancy category X
2.7.4.1.2. iPledge program
2.7.4.1.3. NO refills
2.7.4.1.4. must fill rx in 7 days
2.7.4.1.5. avoid alcohol
2.7.5. anti-inflammatory
2.7.6. hormonal: reduce androgens
3. Pharmacology
3.1. Preferrable Characteristics
3.1.1. <600 Da
3.1.2. Soluble in water and oil
3.1.2.1. water soluble ions and polar mol do not penetrate unless they are very small
3.1.3. High logP
3.2. Glucocorticoids
3.2.1. Immunosuppressive and Anti-inflammatory
3.2.2. Initial high dose and then reduce
3.2.3. Application >2x/d does not improve response
3.3. Intralesional
3.3.1. Preparations (prolonged action)
3.3.1.1. triamcinolone acetonide
3.3.1.2. triamcinolone hexacetonide
3.3.1.3. fluorocinolone
3.3.1.3.1. causes perioral dermatitis and rosacea
3.3.2. Therapeutic Use
3.3.2.1. SEREVE illness
3.3.2.2. allergic contact dermatitis to plants
3.3.2.3. life threatening vesiculobollous dermatoses
3.3.3. SE from long term use
3.3.3.1. psychiatric problems
3.3.3.2. cataracts
3.3.3.3. myopathy
3.3.3.4. osteoporosis
3.3.3.5. avascular bone necrosis
3.3.3.6. glucose intolerance (overt DM)
3.3.3.7. HTN
3.3.4. Toxicity from chronic use
3.3.4.1. atrophy
3.3.4.2. striae
3.3.4.3. telangiectasias: small dilated blood vessels in mucus membrane
3.3.4.4. purpura
3.3.4.5. acne
3.4. Retinoids
3.4.1. Classes
3.4.1.1. 1st Generation
3.4.1.1.1. Retinol
3.4.1.1.2. Tretinoin
3.4.1.1.3. Sotretinoin
3.4.1.1.4. Alitretinoin
3.4.1.2. 2nd Generation (aromatic)
3.4.1.2.1. Acitretin
3.4.1.3. 3rd Generation (arotinoids)
3.4.1.3.1. Tazarotene
3.4.1.3.2. Bexarotene
3.4.1.4. Adapalene has retinoid like properties but does not fall into any class of retinoid
3.4.1.4.1. derivative of naphotic acid
3.4.1.4.2. similar efficacy to tretinoin
3.4.1.4.3. less stable in sun
3.4.1.4.4. less irritating
3.4.1.5. Oral Retinoids
3.4.1.5.1. Isotretinoin
3.4.2. MOA
3.4.2.1. compounds of retinol that exhibit Vitamin A activity
3.4.2.2. activates RARs and RXRs and affects gene expression
3.4.2.3. gene products responsible for pharmacologic effect and SE
3.4.3. Therapeutic use
3.4.3.1. inflammatory skin disorders
3.4.3.2. skin malignancies
3.4.3.2.1. treat premalignant skin cancer (isotretinoin)
3.4.3.3. hyperproliferative disorders
3.4.3.4. photoaging
3.4.3.5. keratinization
3.4.3.6. enhance penetration of topical meds
3.4.4. SE
3.4.4.1. greater SE seen in 1st and 2nd generation
3.4.4.2. xerosis
3.4.4.3. epistaxis
3.4.4.4. conjunctivitis
3.4.4.5. hair loss
3.4.5. Toxicity
3.4.5.1. can affect: vision, cell proliferation, bone growth, immunity, tumor suppression
3.4.5.2. similar to vitamin A intoxication
3.4.6. Teratogenicity
3.4.6.1. pregnancy category X
3.4.6.2. fetal malformations
3.5. Beta Carotene
3.5.1. precursor of vitamin A
3.5.2. in green and yellow veggies
3.5.3. decreases production of free radicals
3.5.4. Clinical Uses...
3.5.4.1. reduces photosensitivity in pts with erythropoetic protoporphyria
3.5.4.1.1. deficiency of ferrochelatase leading to high levels of protoporphyria
3.6. Photochemotherapy
3.6.1. Chemistry Principles...
3.6.1.1. UV C doesn't penetrate
3.6.1.2. UV B 290-320 nm
3.6.1.2.1. most erythrogenic and melanogenic
3.6.1.2.2. sunburn / tanning
3.6.1.2.3. skin cancer
3.6.1.2.4. photoaging
3.6.1.3. UV AI 320-340 nm and UV AII 340-400 nm
3.6.1.3.1. 1000x less erythrogenic than UVB
3.6.1.3.2. photoaging and photosensitivity diseases
3.6.1.3.3. enhances UVB induced erythema
3.6.1.3.4. increase risk for skin cancer
3.6.1.4. visible light 400-800 nm
3.6.2. Phototherapy...
3.6.2.1. Using UVB or High dose UV AI
3.6.2.1.1. Monitor: phenothiazenes, thiazides, sulfonamides, NSAIDs, sulfonylureas, tetracyclines, benzos
3.6.2.2. PUVA: psoralens and UVA chemotherapy
3.6.2.2.1. vitiligo
3.6.2.2.2. psoriasis
3.6.2.2.3. cutaneous T cell lymphoma
3.6.2.2.4. atopic dermatitis
3.6.2.2.5. alopecia
3.6.2.2.6. lichen planus
3.6.2.2.7. urticaria pgmentosa
3.6.2.2.8. promotes melanogenesis in normal skin
3.6.2.2.9. PO administration 8-methylpsoralen followed by UVA
3.7. Sunscreen
3.7.1. For UVA
3.7.1.1. avobenzene
3.7.1.2. oxybenzone
3.7.1.3. titanium dioxide
3.7.1.4. zinc oxide
3.7.2. SPF: the time a person w/ sunscreen can be exposed to the sun before getting sunburn compared to a person w/o sunscreen
3.8. Capsaicin
3.8.1. neuralgia
3.8.2. diabetic neuropathy
3.8.3. arthritis pain
4. Atopic Dermatitis/Eczema
4.1. Overview
4.1.1. chronic relapsing disease that usually begins in infancy or childhood
4.1.2. Triad: atopic dermatitis + asthma + allergic rhinitis
4.1.3. Epidemiology
4.1.3.1. mostly affects children
4.1.3.2. common characteristics: low socioeconomic status, FH, urban area, smaller family
4.1.4. Pathophysiology
4.1.4.1. genetic predisposition
4.1.4.2. initial mechanism unknown
4.1.4.3. Increased IgE
4.1.4.4. S. Aureus colonization
4.1.4.5. skin barrier dysfunction
4.1.4.6. transepidermal water loss
4.2. Clinical Presentation
4.2.1. most cases before 5 years old
4.2.2. initial presentation is facial rash
4.2.3. spares diaper and nose region
4.2.4. rash can include...
4.2.4.1. papules
4.2.4.2. vesicles
4.2.4.3. oozing vesicles
4.2.5. Signs and Symptoms
4.2.5.1. xerosis
4.2.5.2. lichenification (thickened leathery skin)
4.2.5.3. bleeding
4.2.5.4. secondary bacterial infections
4.3. Treatment
4.3.1. Non-pharmacological
4.3.1.1. bathe in lukewarm water 5 min 1-2x/d
4.3.1.1.1. bath > shower
4.3.1.2. bathing 2x/d during flares enhances topical therapy and debrides
4.3.1.3. mild liquid cleansers
4.3.1.3.1. cetaphil
4.3.1.4. Moisturizers
4.3.1.4.1. DO NOT apply to a dressing
4.3.1.4.2. avoid alcohol containing products
4.3.1.4.3. Occlusives are most effective
4.3.1.5. Minimize scratching
4.3.1.6. Minimize triggers
4.3.1.7. Avoid extreme temperatures
4.3.1.7.1. keep home cool with low humidity
4.3.1.8. Treat weeping lesions
4.3.1.8.1. astigents
4.3.2. Pharmacology
4.3.2.1. First Line Therapy...
4.3.2.1.1. Topical corticosteroids
4.3.2.2. Second Line...
4.3.2.2.1. Topical calcineurin inhibitor
4.3.2.3. PO corticosteroids
4.3.2.3.1. short courses for severe
4.3.2.3.2. intensify topical steroids and hydration to minimize rebound flares
4.3.2.4. Phytotherapy
4.3.2.4.1. alt for moderate to severe
4.3.2.4.2. UV therapy
4.3.2.4.3. UV + topical ointment
4.3.2.4.4. psoralens + UVA
4.3.2.5. Coal tar
4.3.2.5.1. ointment, cream, gel, shampoo
4.3.2.5.2. sheds dead cells for top layer to delay growth of new cells and decrease pruritus

