1. Pain out of proportion and pain with passive stretching of muscle.
2. E=Exposure
3. If treatment is delayed surgical correction is the only choice
4. Management: • non operative: remove constructive dressings( casts, splints) and elevate the limb at the level of the heart . • Operative : urgent fascitomy, 48-72h post-op wound closure with or without necrotic tissue debridement .
5. Treatment : serial casting
6. Talipes equinovarus ( Club foot )
6.1. Flection and inversion of the foot
7. Difinition : avascular necrosis of femoral head in children
8. Look for Source of Bleeding
9. Jaw Thrust And Chin Lift
10. CT scan , MRI , Arthrography , Arthrocentesis , Arthroscopy , and bone scan can be used in some cases
11. Treatment
11.1. Pavlik harness
11.2. Hip spica cast
11.3. Open reduction
12. Developmental dysplasia (dislocation) of the hip (DDH)
12.1. Physical examination
12.1.1. Barlow's test
12.1.2. Ortaloni's test
12.2. Investigation
12.2.1. US
13. History
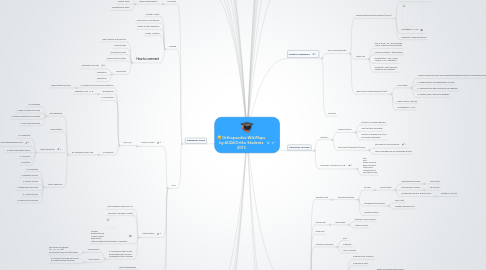
14. Pediatric Orthopaedics
14.1. Hip & foot pathology
14.1.1. Slipped capital femoral epiphysis (SCFE)
14.1.1.1. Difinition : seperation of the epiphysis From the head of the femur
14.1.1.2. Investigation : x-ray
14.1.1.3. Treatment : stabilize with nail
14.1.2. Septic hip
14.1.2.1. Sign & symp : cry , poor feeding , fever, inability to move the hip
14.1.2.2. Common bacteria : staph aureus
14.1.2.3. Investigation : CBC , blood culture , x-ray , aspiration
14.1.2.4. Treatment : open the joint , irregation and antibiotic
14.1.3. Legg-Calvé-Perthes disease (LCPD)
14.1.3.1. Four Stages
14.1.3.1.1. 1-Femoral head becomes more dense with possible fracture of supporting bone
14.1.3.1.2. 2-Fragmentation and reabsorption of bone
14.1.3.1.3. 3- Reossification when new bone has regrown
14.1.3.1.4. 4-Healing, when new bone reshapes.
14.1.3.2. Signs & symp : hip pain
14.1.3.3. Investigations : x-ray
14.2. Fractures
15. Orthopaedic Oncology
15.1. Statistics
15.1.1. primary tumors
15.1.1.1. Posterior Cruciate Ligament
15.1.1.2. most of them are benign
15.1.1.3. must be managed only by an oncologist orthopedic
15.1.2. secondary (Metastatic) tumors
15.1.2.1. the majority of bone tumors
15.1.2.2. can be managed by any orthopedic doctor
15.2. Important 7 quistions in x-ray
15.2.1. Site Size Effect on bone Bone response Matrix type Cortex erosion Soft tissue mass
16. Spine Surgery
17. Sport Injuries
18. Arthroplasty
19. Orthopaedic Trauma
19.1. Hx and PE
19.1.1. Physical Examination
19.1.1.1. LOOK, FEEL & MOVE
19.1.1.2. Special Tests
19.1.1.3. Neurovascular Exam
19.2. imaging
19.2.1. at least 2 views
19.2.2. Joint Above & Joint Below
19.2.3. Before & After Reduction
19.2.4. 2 sides : bilateral
19.2.5. How to comment
19.2.5.1. Take a history & Physical Ex
19.2.5.2. Personal data
19.2.5.3. The area and view
19.2.5.4. Follow cortical outline
19.2.5.5. description
19.2.5.5.1. Dislocation for joint
19.2.5.5.2. Angulation
19.2.5.5.3. Shortening
19.3. ATLS
19.3.1. Primary Survey
19.3.1.1. A,B,C,D,E
19.3.1.1.1. A=Airway & Cervical Spine Protection
19.3.1.1.2. B=Breathing
19.3.1.1.3. C=Circulation
19.3.1.1.4. D=Disability
19.3.2. Resuscitation
19.3.2.1. Two peripheral large bore IVs
19.3.2.2. Two liters of Ringers Lactate
19.3.2.3. Monitor Blood pressure Urinary output Base deficit Initial Hematocrit/Hemoglobin -unreliable
19.3.2.4. If no response then severe hemorrhage has occurred Immediate blood is needed
19.3.2.4.1. Type specific
19.3.2.4.2. cross match
19.3.3. Secondary Survey
19.3.3.1. after pt stablization
19.3.3.2. look for Dx
19.3.4. Tertiary Survey
19.3.4.1. in 24 hr after stablization
19.3.4.2. look for missing abnormality
20. Foot & Ankle
20.1. Achilles Tendon
20.2. Peroneal Tendons
20.3. Posterior Tibial Tendon Dysfunction (PTTD)
20.4. Foot Disorders
20.5. Fractures
21. Upper Extremities
21.1. Shoulder joint
21.1.1. Shoulder problems
21.1.1.1. RC tear
21.1.1.1.1. special tests
21.1.1.2. Impingement syndrome
21.1.1.2.1. Neer's test
21.1.1.2.2. Hawkins-Kennedy test
21.1.1.3. Shoulder trauma
21.2. Elbow joint
21.2.1. Dislocation
21.2.1.1. Posterior most common
21.2.1.2. Anterior is rare
21.3. wrist joint
21.4. Common complains
21.4.1. Pain
21.4.2. Instability
21.4.3. Loss of motion
21.5. Fractures
21.5.1. Clavicle Fx
21.5.1.1. Proximal most common
21.5.1.2. Common in child
21.5.1.3. P/E & Radiology
21.5.1.3.1. Check for brachial plexus injury
21.5.1.3.2. X-ray, AP chest
21.5.1.4. Rx
21.5.1.4.1. Proximal & Middle
21.5.1.4.2. Distal
21.5.1.5. Complications
21.5.1.5.1. Shoulder stiffness
21.5.1.5.2. brachial plexus injury
21.5.1.5.3. Pneumothorax
21.5.2. Proximal Humral Fx
21.5.2.1. P/E & Radiology
21.5.2.1.1. Neurovascular Examination
21.5.2.2. Rx
21.5.2.2.1. Treat osteoprosis
21.5.2.2.2. Undisp.
21.5.2.2.3. Disp.
21.5.2.3. Complications
21.5.2.3.1. AVN
21.5.2.3.2. Axillary nerve palsy
21.5.2.3.3. Post-trumatic arthritis
22. Acute Compartment Syndrome
22.1. Surgical ER. causes:after significant trauma,ischemic injury, prolonged limb compression or surgery.
23. Orthopadeic Basic Sciences
23.1. New Idea
23.2. New Idea
23.3. New Idea
23.4. New Idea
23.5. New Idea
24. Knee joint
24.1. Knee injuries
24.1.1. fracture
24.1.1.1. Tibial Plateau Fractures
24.1.1.1.1. Produced by varus or valgus forces combined w/axial loading which drives femoral condyles into tibial plateau
24.1.1.2. Tibial Spine & Tuberosity Fractures
24.1.1.3. Femoral Condyle Fractures
24.1.1.4. Patella Fracture
24.1.2. ligament injuries
24.1.2.1. Ligamentous & Meniscal Injuries
24.1.2.1.1. Collateral ligament injury
24.1.2.1.2. Meniscal tears
24.1.2.2. Anterior Cruciate Ligament
24.1.2.2.1. ACL tear >PCL tear
24.1.3. dislocation
24.1.3.1. Knee Dislocation:
24.1.4. inflammation
24.1.4.1. Patellar Tendonitis
24.1.4.2. osteoarthritis
24.1.5. Quadriceps/Patellar Tendon Rupture
24.1.5.1. Patella Dislocation
24.1.6. Chondromalacia Patellae
