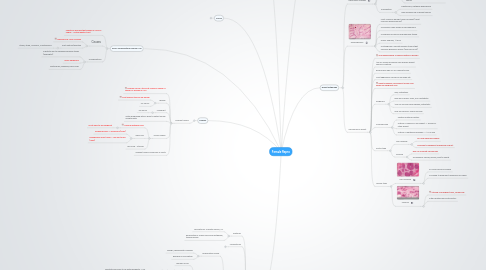
1. Vagina
1.1. Vaginitis
1.1.1. Trichomonas vaginalis
1.1.1.1. Can be asymptomatic
1.1.1.2. watery gray- green discharge with a foul odor.
1.1.2. Candida albicans
1.1.2.1. Can be asymptomatic
1.1.2.2. Causes itching and a curdy white discharge
1.1.2.3. Present in 5% women
2. Cervix
2.1. Anatomy
2.1.1. Endocervical canal
2.1.1.1. Columnar-mucus
2.1.2. Transitional zone
2.1.2.1. Squamo-columnar junction
2.1.2.1.1. Most likely region for cervical dysplasia
2.1.3. Ectocervix
2.1.3.1. Squamos
2.2. Cervical Neoplasia
2.2.1. Risk factors
2.2.1.1. i. Early age at first intercourse. ii. Multiple sexual partners. iii. Smoking iv. HIV
2.2.2. HPV: causes squamous neoplasms of cervix
2.2.2.1. Low risk: 6, 11 -> Condylomas (benign)
2.2.2.2. High Risk: 16, 18, 31 -> Cervical carcinoma
2.2.2.3. Both low and high found in dysplastic lesions
2.2.3. Condyloma
2.2.3.1. Wart projections
2.2.3.2. Coilistic change: viral induced cytopathic change
2.2.3.2.1. Raisonid cells
2.2.3.2.2. Empty cytoplasm, dark wrinkly nucleus
2.2.3.3. Low grade dysplasia -> DOESN'T progress to cancer
2.2.4. Cervical dysplasia
2.2.4.1. Pre-malignant condition
2.2.4.1.1. May progress to carcinoma
2.2.4.1.2. Most spontaneously regress
2.2.4.2. Scoring
2.2.4.2.1. CIN 1: < 1/3 epithelial involvement
2.2.4.2.2. CIN 2: 1/3 - 2/3
2.2.4.2.3. CIN 3: 2/3 - complete
2.2.4.2.4. CIN 3 = carcinoma in situ (CIS)
2.2.4.2.5. PAP Smear -> Scoring is based on degree of dysplasia of individual cells.
2.2.5. Cervical squamous cell carcinoma
2.2.5.1. Can be in situ or invasive
2.2.5.2. Gross: Granular and hemmorhagic
3. Uterus
3.1. Anatomy
3.1.1. Myometrium: Smooth muscle, CT
3.1.2. Endometrium: simple columnar epithelium, tubular glands
3.2. Myometrium
3.2.1. Uterine Leiomyomas: fibroid
3.2.1.1. Benign tumors
3.2.1.2. Gross: whorls (spirals) of smooth muscle
3.2.1.3. Possible cause: excessive estrogenic stimulation
3.2.1.4. Symptoms
3.2.1.4.1. › Pain and pressure on the urinary bladder › Impaired fertility › Profuse bleeding during menstruation › Problems during pregnancy including spontaneous abortion.
3.2.2. Leiomyosarcoma
3.2.2.1. Malignant smooth muscle tumor from myometrium
3.2.2.2. Generally don't develop from existing leiomyoma
3.2.2.3. Can metastasize
3.3. Endometrium
3.3.1. Endometrial Polyps
3.3.1.1. Benign, hyperplastic changes
3.3.1.2. Bleeding is a symptom
3.3.2. Endometrial Carcinoma
3.3.2.1. Women 55-60
3.3.2.2. Associated with obesity, hypertension, infertility
3.3.2.2.1. Infertility has more to do with neloparity. = No kids = Never a break from menstrual cycle. Excess Estrogen.
3.3.2.3. Symptom: Post-menopausal bleeding
3.3.2.4. May develop from endometrial hyperplasia
3.3.3. Endometriosis
3.3.3.1. Presence of endometrial glands/stroma outside uterus.
3.3.3.2. Location: descending frequency
3.3.3.2.1. 1. The ovaries. 2. The uterine ligaments. 3. The rectovaginal septum. 4. The pelvic peritoneum. 5. Laparotomy scars. 6. Rarely involves the umbilicus, vagina, vulva, or appendix. 7. Muscular wall of uterus
3.3.3.3. Potential causes
3.3.3.3.1. 1. Regurgitation of menstrual backflow through the fallopian tubes
3.3.3.3.2. 2. Endometrial metaplastic differentiation of epithelial elements covering involved structures.
3.3.3.3.3. 3. Vascular or lymphatic dissemination of endometrial elements.
3.3.3.4. Specific locations
3.3.3.4.1. Adenomyosis Uteri: Endometriosis in muscular wall of the uterus
3.3.3.4.2. Endometriod: chocolate cysts in ovaries
4. Ovaries
4.1. Ovarian tumors
4.1.1. Ovarian cancer: 5th most common cause of cancer of women in USA
4.1.2. Benign
4.1.2.1. Most ovarian tumors are benign
4.1.2.2. 24-45 yrs.
4.1.3. Malignant
4.1.3.1. 40-65 yrs
4.1.4. Often diagnosed late bc hard to detect unless symptomatic
4.1.5. Tumor origins
4.1.5.1. Surface epithelial cells
4.1.5.1.1. Most likely to be malignant
4.1.5.2. Germ cell
4.1.5.2.1. Dysgerminoma = Seminoma (male)
4.1.5.2.2. Endodermal sinus tumor = Yolk sac tumor (male)
4.1.5.3. Sex Cord - Stromal
4.1.6. Ovarian tumors commonly in cysts
5. Pelvic Inflammatory Disease: PID
5.1. Infectious process that begins in vulva or vagina -> entire genital tract
5.2. Causes
5.2.1. Gonococcus: very common
5.2.2. Post-partum/abortion
5.2.2.1. Staph, Strep, Colliform, Clostridium p.
5.3. Complications
5.3.1. Infertility due to damaged fallopian tubes (salpingitis)
5.3.2. Pelvic adhesions
5.3.3. Bacteremia, bleeding, pelvic pain
6. Breast Pathology
6.1. Fibrocystic changes
6.1.1. Extremely common
6.1.2. Likely related to hormone variations, esp. estrogen
6.1.3. Non-proliferative
6.1.3.1. Increased fibrous stroma formation of cysts dilation of ducts
6.1.3.2. Not associated with increased risk of breast cancer
6.1.4. Proliferative
6.1.4.1. Additionally, epithelial hyperplasia
6.1.4.2. may increase risk of breast cancer
6.2. Fibroadenoma
6.2.1. Most common benign tumor of breast (most common before age 30)
6.2.2. Carcinoma rarely arises in fibroadenoma
6.2.3. Composed of fibrous and glandular tissue.
6.2.4. Gross: nodules, 1-15cm
6.2.5. Histologically: delicate fibrous stroma that encloses glandular spaces (and loss of fat)
6.3. Carcinoma of breast
6.3.1. 2nd leading cause of cancer deaths in women
6.3.2. 10% of American women will develop breast cancer in lifetime.
6.3.3. Rare before age 25-30. Peaks at 60yrs
6.3.4. Most aggressive cancers in younger pts
6.3.5. Paget's disease: involvement of skin and nipple by malignant cells
6.3.6. Prognosis
6.3.6.1. size, metastasis
6.3.6.2. 80% 5yr survival: small, non-metastatic
6.3.6.3. 10% 5yr survival: wide spread, metastatic
6.3.6.4. 50% 5yr survival: overall survival
6.3.7. Increased risk
6.3.7.1. Positive maternal history
6.3.7.2. History of cancer in one breast -> 5x risk for other breast
6.3.7.3. History of epithelial dysplasia -> 1.5-2x risk
6.3.8. Ductal type
6.3.8.1. Non-invasive
6.3.8.1.1. 30-50% become invasive
6.3.8.1.2. confined to basement membrane of duct
6.3.8.2. Invasive
6.3.8.2.1. 90% of all breast carcinomas
6.3.8.2.2. Arranged as chords, glands, and/or sheets
6.3.9. Lobular type
6.3.9.1. Non-invasive
6.3.9.1.1. 20-30% become invasive
6.3.9.1.2. Confined to basement membrane of lobule
6.3.9.2. Invasive
6.3.9.2.1. Strands of malignant cells, "indian file"
6.3.9.2.2. Often bilateral and mutlicentric
7. Pregnancy related diseases
7.1. Ectopic pregnancy
7.1.1. Implantation in any site other than uterus
7.1.1.1. Fallopian tubes 90%
7.1.2. Incidence 1/150
7.1.3. Predisposing factors
7.1.3.1. PID -> chronic salpingitis, fallopian tube scarring
7.1.3.2. Peritubal adhesions
7.1.3.3. 50% of causes no apparent tubal abnormalities
7.1.4. Complications
7.1.4.1. Bleeding into fallopian tube
7.1.4.2. Tubal rupture and hemorrhage: doesn't normally occur. Within first 2-6 weeks pregnancy.
7.2. Toxemia of pregnancy
7.2.1. Pre-eclampsia
7.2.1.1. The development of hypertension, proteinuria and edema in the third trimester of pregnancy
7.2.1.2. Typically first pregnancy, ie parity. (5-10%)
7.2.1.3. Tx is Magnesium (prevents progressing to eclampsia)
7.2.2. Eclampsia
7.2.2.1. Pre-eclampsia plus the development of convulsive seizures
7.2.2.2. WHY DOES IT HAPPEN
7.3. Gestational trophoblastic disease
7.3.1. Placenta doesn't develop normally
7.3.2. Caused by proliferation of pregnancy-associated trophoblastic tissue.
7.3.3. Hydatidiform Mole
7.3.3.1. Cystic swelling of chorionic villi
7.3.3.2. Variable degrees of trophoblastic proliferation
7.3.3.3. Increased serum HCG
7.3.3.4. Tx
7.3.3.4.1. Chemotherapy: Invasive moles (10% of moles)
7.3.3.4.2. Track progress using HCG levels
7.3.3.5. Complete type:
7.3.3.5.1. Hydrophobic swelling of all villi
7.3.3.5.2. Diffuse trophoblastic hyperplasia
7.3.3.5.3. Fetal parts rarely present
7.3.3.5.4. Choriocarcinoma precursor
7.3.3.6. Partial type:
7.3.3.6.1. Only some villi undergo hydrophobic swelling
7.3.3.6.2. Focal trophoblastic hyperplasia
7.3.3.6.3. Is not a choriocarcinoma precursor
7.3.4. Choriocarcinoma
7.3.4.1. Dangerous
7.3.4.1.1. Aggressive
7.3.4.1.2. Widely Metastisizing
7.3.4.1.3. High-grade trophoblastic malignancy
7.3.4.1.4. 1/20,000 pregnancies
7.3.4.2. Increased HCG
7.3.4.3. Gross: large, fleshy, and has areas of necrosis and hemorrhage.
7.3.4.4. Histologically: proliferated trophoblastic cells; villi are not present
7.3.4.5. Preceded by these conditions
7.3.4.5.1. 50% Complete Mole
7.3.4.5.2. 25% abortion
7.3.4.5.3. 22% normal pregancy
