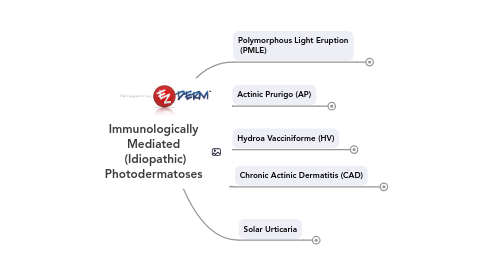
1. Solar Urticaria
1.1. Action Spectrum
1.1.1. Visible light
1.1.2. Positive photo-testing with visible light (e.g., slide projector lamp) is diagnostic value
1.2. Type I Hypersensitivity Reaction
1.3. Clinical Presentation
1.3.1. Wheals start within (up to 30) minutes of sun exposure and last < 24 hours
1.3.2. Usually Females during 4th and 5th decade of life
1.3.3. May progress to anaphylactoid reaction
1.4. Associations
1.4.1. Atopic Dermatitis (up to 50%)
1.4.2. Erythropoetic Protoporphiria (EPP)
1.4.3. Lupus Erythematous
1.4.4. Medications
1.5. Therefore, test for LE and EPP in patients with solar urticaria
1.5.1. Negative test results seen in PMLE, AP, and CAD
1.6. Variants
1.6.1. Fixed SU
1.6.1.1. Limited to specific area on the body
1.6.2. Drug-Induced SU
1.6.2.1. Chlorpromazine
1.6.2.2. Tetracycline
1.7. Therapy
1.7.1. Photoprotection, Antihistamines, Low-Dose UVA, PUVA,
1.7.2. IVIG (in difficult cases)
2. Chronic Actinic Dermatitis (CAD)
2.1. 3 Main Criteria:
2.1.1. Reduction in the MED to UVA, UVB and/or visible light
2.1.1.1. The hallmark of CAD is a lowered MEDB
2.1.1.1.1. Only CAD has lowered MEDB, distinguishing it from photoallergic contact dermatitis
2.1.1.1.2. So any board question with lower MEDB is most likely to be related to CAD
2.1.2. Photo-distribution
2.1.3. Pathology c/w AD with/without CTCL-like changes
2.2. Action Spectrum
2.2.1. UVB
2.3. DTH Type IV reaction (i.e., photoallergic)
2.4. Clinical Presentation
2.4.1. Usually men > 50 y/o (all races)
2.4.2. Initial symptom: persistent erythema of the face
2.4.3. Allergic and/or photoallergic contact dermatitis commonly coexist with CAD and often precedes the onset of photosensitivity
2.4.4. Positive patch testing
2.4.4.1. Sesquiterpene lactone mix
2.4.4.2. Compositae in UK patients
2.5. Treatment
2.5.1. Photoprotection, Allergen Avoidance, Azathioprine, CYS-A, MMF, Low Dose PUVA, topical Tacrolimus
2.6. CAD in younger individuals infected with HIV has recently been described
3. Hydroa Vacciniforme (HV)
3.1. Rare, chronic photodermatosis
3.2. Clinical Presentation
3.2.1. Occurring predominantly during the childhood (3-15 y/o; remits in adolescence)
3.2.2. Umbilicated vesicles in sun-exposed areas
3.2.3. appear within 30 minutes to 2 hours after sun exposure
3.2.4. Heal with vacciniform (varioliform) scars
3.2.5. May be accompanied by keratoconjuctivitis, photophobia, and constitutional symptoms
3.2.6. Boys tend to have longer course
3.3. Action Spectrum
3.3.1. UVA (most commonly)
3.4. Treatment
3.4.1. Photoprotection, NB-UVB, PUVA
3.5. Hydroa Vacciniforme-Like Lymphoma
3.5.1. Severe forms of HV-like eruptions have been linked with an aggressive type of T-cell lymphoma
3.5.2. EBV-associated
3.5.3. mainly found in children from Asia and Latin America
4. Actinic Prurigo (AP)
4.1. Two variants
4.1.1. General Variant (Hutchinson’s Summer Prurigo):
4.1.1.1. May present a persistent variant of PMLE that occurs in genetically susceptible individuals
4.1.1.2. starts in childhood and resolves in adolescence
4.1.1.3. Girls > Boys
4.1.1.4. Usually European Countries (temperate climate)
4.1.1.5. Worse in summer (rarely in other seasons)
4.1.2. Familial PMLE of Native Americans
4.1.2.1. Girls = Boys
4.1.2.2. Persists into adulthood (F>M)
4.1.2.3. Skin photo-types IV and V
4.1.2.4. Occurs year-round
4.2. Clinically different than PMLE:
4.2.1. HLA DRB1*0407 marker distinguishes it from PMLE
4.2.2. Can involve photo-protected skin areas
4.2.3. Intensely pruritic, excoriated/lichenified papules and nodules with hemorrhagic crust that last longer than PMLE
4.2.4. Persists into winter
4.2.5. Cheilitis and Conjunctivitis are common (use eye protection)
4.3. Treatment: Thalidomide, Sun Glasses and Photoprotection, NB-UVB
5. Polymorphous Light Eruption (PMLE)
5.1. UVA is the most common action spectrum
5.2. Reproduction of lesions by photo-testing is of diagnostic value
5.3. Normal MED A/B
5.4. Skin phototypes I-IV
5.5. F>M
5.6. DTH response (Type IV Hypersensitivity) to a photo-induced antigen.
5.7. Clinical Presentation
5.7.1. Usually 2nd-3rd decade of life
5.7.2. Spring and early summer months in temperate climates
5.7.3. Presents minutes to hours (rarely days) after exposure to sunlight or artificial UVR (even visible light
5.7.4. Exclusively photo-distributed
5.7.5. Monomorphic papules, vesicles, and EM-like targetoid lesions
5.7.6. Eczematous and papular forms are the most common
5.7.7. No relation to a photo-sensitizing medication
5.7.8. Self limited due to “UV Hardening”: lasts for one to several days (occasionally weeks)
5.8. Treatment:
5.8.1. Sun avoidance, sunscreens and sun-protective clothing.
5.8.2. Sever cases: UV hardening, antimalarials, and prednisone.
