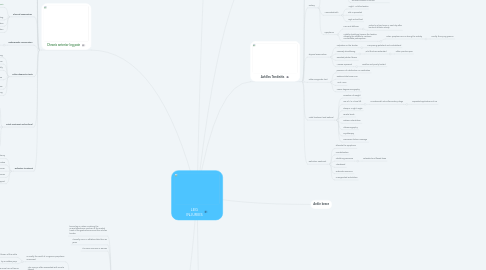
1. Chronic anterior leg pain
1.1. refers to
1.1.1. pain
1.1.1.1. between
1.1.1.1.1. knee
1.1.1.1.2. Ankle
1.2. the diagnosis differential
1.2.1. include
1.2.1.1. stress fractures
1.2.1.2. periostitis
1.2.1.3. tibialis posterior syndrome
1.2.1.4. etc
1.3. Mechanism of injury
1.3.1. overuse
1.3.2. new activity
1.3.3. alteration in terrain
1.3.4. shoes
1.3.5. biomechanical alterations
1.3.5.1. for example
1.3.5.1.1. hyperpronation of the foot
1.4. Symptoms
1.4.1. pain
1.4.1.1. in
1.4.1.1.1. distal lateral
1.4.1.1.2. anterior lateral
1.4.1.1.3. anterior surface
1.4.1.1.4. medial zone
1.4.2. swelling
1.4.3. tense sensation
1.4.4. tissue swelling
1.4.5. paresthesia
1.4.6. hypesthesia
1.5. Physical examination
1.5.1. locate
1.5.1.1. tenderness areas
1.5.1.2. bone disorders
1.5.1.3. soft tissue alterations
1.5.2. muscle testing
1.5.3. palpation
1.5.4. observation
1.6. Radiographic examination
1.6.1. radiographs
1.6.1.1. ant-post
1.6.1.2. lateral
1.6.1.3. oblique
1.7. Other diagnostic tests
1.7.1. radionuclide bone scanning
1.7.2. triple-phase bone scan
1.7.3. Identify
1.7.3.1. hot spots
1.7.4. Excercise
1.7.4.1. pre
1.7.4.2. post
1.7.5. intracomportamental pressures
1.7.6. muscle testing
1.8. Initial Treatment and Referral
1.8.1. decrease
1.8.1.1. pain
1.8.1.2. inflammation
1.8.2. use of
1.8.2.1. ice
1.8.2.2. ultrasonography
1.8.2.3. current galvanic
1.8.2.4. medication
1.8.2.5. air support
1.8.3. refered to
1.8.3.1. orthopedic surgeon
1.8.3.2. podiatrist
1.9. Definitive treatment
1.9.1. fasciotomy
1.9.2. modify activities
1.9.3. streching excercise
1.9.4. strengthening excercise
1.9.5. arch support
2. Gastrocnemius Strain (Tennis Leg)
2.1. tennis leg is a strain involving the musculotendinous junction of the medial head of the gastrocnemius and the achilles tendon
2.2. it usually occur in athletes older than 30 years
2.3. It's more common in women
2.4. History
2.4.1. mechanics of injury
2.4.1.1. is usually the result of a vigorous propulsive movement
2.4.1.1.1. plantar flexion of the ankle
2.4.1.1.2. by a sudden jump
2.4.1.2. This injury is often associated with muscle fatigue
2.4.1.2.1. for playing one more hour of tennis
2.4.1.3. the injury occurs after a strain in the ankle or a sprain
2.4.1.3.1. either by a relative weakness with stiffness in the calf
2.4.1.4. occasionally the injury occus en two parts
2.4.1.4.1. a minor strain that is ignored, followed minutes later by complete rupture of the musculotendinous unit
2.4.1.4.2. minutes later by complete rupture of the musculotendinous unit
2.4.2. Symptoms
2.4.2.1. the athlete feels or hears a click in the medial part of the calf at the top
2.4.2.1.1. the patient believes that he was hit in the calf with the racket or the tennis ball
2.4.2.2. The wound is painful
2.4.2.2.1. The spasm of the calf musculature occurs quickly, flexing the foot plantar
2.4.2.3. swelling and ecchymosis are not seen in the first hours
2.4.2.3.1. after 24 to 48 hours it is important to have immediate medical attention
2.5. weeks after the appearance of the injury
2.6. Physical Examination
2.6.1. the most frequent feature
2.6.1.1. the most frequent feature
2.6.2. swelling and ecchymosis is more frequent
2.6.2.1. distal part of the injury, which can affect the ankle to the foot
2.6.3. movement is limited and the athlete walks on the toes
2.6.4. When the athlete's knee is extended, passive dorsiflexion in the ankle and plantar flexion act against resistance
2.6.4.1. there will be pain in the side of the injury
2.6.4.1.1. it is possible palpal a defect in the muscle
2.6.4.1.2. but this is quickly filled with blood
2.7. Radiographic Examination
2.7.1. The radiographic study is not required
2.7.2. Other Diagnostic Test
2.7.2.1. It is no necessary 7
2.8. Initial treatment
2.8.1. If the athlete is seen within a few hours of the injury, the foot should be placed in neutral position
2.8.1.1. And maintain the neutral position with a plaster splint subsequently packaged
2.8.1.2. The gastrocnemius tightens the surrounding fascia and this disables the continuation of the hemorrhage
2.8.2. Efforts to regain ankle motion must be started at 24 hors after injury
2.8.2.1. active and passive stretching is very important
2.8.2.2. it is faster to put the athlete to walk forcefully even if it is uncomfortable for him
2.8.3. weeks after the appearance of the injury
2.8.3.1. The patient presents the ankle in plantar flexion due to a spasm located in the part of the calf.
2.8.3.2. The foot presents a chronic inflammation
2.8.3.3. a compression is made from the fingers to the knee
2.8.4. when it is an unattended case
2.8.4.1. March that are not heavy should be used during the first days after the initial visit
2.8.4.2. until the patient is able to walk with a gait heel and toes painless
2.9. Definitive Treatment
2.9.1. recover muscle strength of the calf
2.9.2. the athlete will perform co-contraction stretches with the extended leg and using a towel as a sling
2.9.3. Male movements will be made until the athlete returns to stand and follow his daily activities
3. Ankle brace
4. Radiographic Examination
4.1. Not necessary
4.2. In chronic case
4.2.1. lateral view
5. Achilles Tendon Strain (RUPTURE)
5.1. Involves one of the largest tendons in the body
5.1.1. U
5.2. History
5.2.1. Mechanism of injury
5.2.1.1. It is accompanied by a click or an audible snap
5.2.1.2. It's an impulse with the front part of the foot
5.2.1.2.1. It can also occur as a result of unexpected or forced dorsiflexion of the ankle with plantar flexion
5.2.1.2.2. Demonstrates the extent and location of the tendon disruption
5.2.2. Symptoms
5.2.2.1. Is the sensation of being hit in the tendon region
5.3. Other Diagnostic Tests
5.3.1. Magnetic resonance
5.4. Physical Examination
5.4.1. Loss of plantar flexion strength
5.4.2. Careful palpation
5.4.2.1. Reveals a loss of continuity in the tendon
5.4.3. Bleeding and inflammation can be important
5.4.4. Sensitivity and pain with movement are present
5.5. Initial Treatment
5.5.1. Must be in a position of plantar flexion assisted by gravity
5.5.2. Ankle
5.5.2.1. A posterior plaster splint
5.6. Definitive Treatment
5.6.1. The direct approach of the tendon fibers
5.6.1.1. Is necessary to preserve the length / tension ratio
5.6.2. Be left to the treating orthopedist
5.6.3. Surgical or non-surgical treatment is used
5.6.4. Immobilization in plaster or corset
5.6.5. Rehabilitation
6. Acute compartment syndromes
6.1. what is?
6.2. history
6.2.1. mechanism of injury
6.2.1.1. tendon ruptures
6.2.1.2. muscle strain
6.2.1.3. contusions
6.2.1.4. acute overuse
6.2.2. symptoms
6.2.2.1. hallmark (pain)
6.2.2.2. paresthesias
6.3. physical examination
6.4. diagnostic test
6.4.1. confirmed by
6.4.1.1. measurement intracompartmental pressure
6.5. initial treatment
6.5.1. rest
6.5.2. rice
6.6. referral
6.6.1. if pressure exceeds 30 mmHg
6.6.2. symptoms of neurvascular impairment
6.7. definitive treatment
6.7.1. if rest and ice dont improve
6.7.2. is necessary when it exceeds 30mmHg
6.7.3. associated with neurovascular impairment
7. Achilles Tendinitis
7.1. It´s common in athletes
7.1.1. It can be in a long term a disability and later a rupture
7.1.1.1. Chronically inflamed partial rupture, stenosis of surrounding soft tissues and calcification of the tendon
7.2. Associated problems
7.2.1. The injury is always seen when its chronic
7.2.2. The rehab is a time-consuming and frustrating process
7.2.2.1. Difficult to supervise and in a high-intensity athlete the injury seems prevalent
7.3. History
7.3.1. Mechanism of injury
7.3.1.1. Result of unaccustomed activity such as hill running
7.3.1.2. Changing of heel height on the running shoe or repetitive jumping.
7.3.1.3. A poorly fitting skating boot or improperly tied ribbons on a ballet pointe shoe.
7.3.1.4. Direct trauma like pressure from the top of the heel counter of a shoe
7.3.2. Associated with
7.3.2.1. "Tight" Achilles tendon
7.3.2.2. Flat or pronated
7.3.2.3. High-arched foot
7.3.3. Symptoms
7.3.3.1. Pain and stiffness
7.3.3.1.1. Noted in a few hours or next day after bouts of athletic activity
7.3.3.2. Initially, stretching loosens the tendon, allowing the athlete to continue comfortable participation.
7.3.3.2.1. Later, symptoms occur during the activity
7.4. Physical examination
7.4.1. Palpation on the tendon
7.4.1.1. Comparing ipsilateral and contralateral
7.4.2. Passively dorsiflexing
7.4.2.1. Whit the knee extended
7.4.2.1.1. Often produce pain
7.4.3. Resisted plantar flexion
7.4.4. Masses represent
7.4.4.1. Swollen and poorly healed.
7.5. Other Diagnostic test
7.5.1. presence of calcification or ossification
7.5.2. Radionuclide bone scan.
7.5.3. "Hot" scan
7.5.4. Lesser degree sonography
7.6. Initial treatment and Referral
7.6.1. Cessation of weight
7.6.2. Use of 1/2 in heel lift
7.6.2.1. Nonsteroidal anti-inflammatory drugs
7.6.2.1.1. Repeated applications of ice
7.6.3. Sleep in a right- angle
7.6.4. Tensile loads
7.6.5. Galvanic stimalution
7.6.6. Ultrasonography
7.6.7. Cryotherapy
7.6.8. Transverse friction massage
7.7. Definitive Treatment
7.7.1. alleviate the symptoms
7.7.2. Immobilization
7.7.3. Stretching exercices
7.7.3.1. extended and flexed-knee
7.7.4. Theraband
7.7.5. Isokinetic exercices
7.7.6. Unsupported ambulation
