1. Mood Disorders
1.1. high or low moods that are prolonged, painful, disruptive, or inappropriate for the situation
1.2. Major Depressive Disorder = includes: depressed mood, loss of interest in things that used to be important, loss of appetite, fatigue or insomnia, agitation, and feelings of worthlessness or guilt, or when severe: loss of contact with reality.
1.2.1. Diagnosis of major depression occurs with long-lasting or recurring depressive episodes.
1.2.2. >could lead to both subjective distress and impairment.
1.2.3. Heritable component for depression; but it’s likely that genes interact with experience to produce depression or, conversely, to produce resistance to depression.
1.3. Manic Episode: opposite of a depressive episode
1.3.1. -elated -energetic -powerful/grandiose,(don’t need sleep) -very impulsive and risky, (little thought of consequences/ feeling that things can’t possibly go wrong) -loss of contact with reality=person believes that they are supernatural/royalty/smarter than everyone else in the world OR some feel very irritable and angry.
1.3.2. >might not have ‘subjective distress’ associated with it, but it could certainly lead to impairment
1.4. Hypomanic Episode is a milder version of a manic episode
1.4.1. definitely more ‘up’ than normal but doesn’t include any delusions or really extreme behaviors: people may be more productive than usual, or more creative and excitable. It isn’t a disorder, all by itself, and people report that it feels pretty great.
1.5. Bipolar Disorder- alternate two ends of a spectrum or two extremes (mania and depression) in the same person at different times
1.5.1. Bipolar I: manic episodes, and may also include depressive episodes or mild depressive symptoms that alternate with the manic episodes.
1.5.2. Bipolar II: hypomanic episodes as well as depressive episodes
1.5.3. twin studies have revealed a much stronger association between identical twins for bipolar, compared to major depression, and this suggests a stronger genetic role for bipolar disorder.
1.6. Variations
1.6.1. Dysthymia is a milder chronic depression
1.6.2. Cyclothymia is a milder chronic version of Bipolar
1.6.3. Specific versions of depression associated with major hormone fluctuations
1.6.3.1. e.g.) Postpartum depression
1.6.4. >variations suggest that there are definite biological triggers for mood episodes that are separate from how good or bad your life experience might be
2. Schizophrenia
2.1. experience distortion or disruption to their experience of reality (psychosis)
2.1.1. may hear or see or feel things that aren’t there, develop associations between things that shouldn’t be associated; Normal patterns of reactions become disorganized
2.2. Positive Symptoms (normal people lack, but patients have ABUNDANCE of)
2.2.1. Hallucinations- affect your perception; see, hear, feel, or even taste and smell things that aren’t there or you will experience distortions of your perception
2.2.1.1. (similar effect can be produced with hallucinogenic drugs, so make sure to rule that out when diagnosing someone with schiz)
2.2.2. Delusions- beliefs that are improbable or impossible, and sometimes emerge because of weird or seemingly random associations that the person makes
2.3. Negative Symptoms (normal people have, patients LACK)
2.3.1. absence of emotional reactions (flat affect)
2.3.2. absence of normal speech→ (most extreme version) is complete catatonia where the patient seems zombie-like, or unresponsive
2.4. With current treatments, people with positive symptoms seem to respond better to treatment and have a better likelihood of recovering and leading a reasonably normal life. People with more negative symptoms seem to have a poorer long-term prognosis.
2.5. With current treatments, people with positive symptoms seem to respond better to treatment and have a better likelihood of recovering and leading a reasonably normal life. People with more negative symptoms seem to have a poorer long-term prognosis.
2.6. Biological component
2.6.1. -Hypofrontality occurs- shrinkage of the cortex, and a lack of activation in the frontal lobes
2.6.2. -Enlarged ventricles when you look at an MRI of the brain- ventricles are the areas where cerebrospinal fluid flows through the brain, and those areas get bigger when other areas of the brain shrink.
2.6.3. >degree of abnormality in the brain is correlated with the severity of symptoms BUT it isn’t clear whether the brain abnormalities cause the symptoms or are a consequence of the disorder
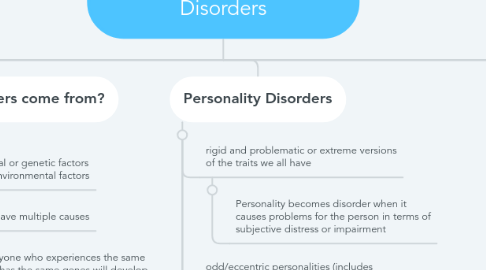
3. Where do disorders come from?
3.1. there are interactions between the biological or genetic factors and the learning or environmental factors
3.1.1. disorders can have multiple causes
3.1.1.1. not everyone who experiences the same thing or has the same genes will develop the same disorders
3.2. Psychoanalytic Perspective
3.2.1. disordered behavior as a consequence of the unconscious mind protecting the conscious mind, or as some failure of the ego to balance between the id and superego.
3.3. Humanistic Perspective
3.3.1. failing to improve or achieve the ideal version of the self
3.4. Biological Perspective
3.4.1. focus on genetic and physiological explanations for disorders
3.5. Learning Perspective
3.5.1. based on classical and operant conditioning explanations for behavior
4. Personality Disorders
4.1. rigid and problematic or extreme versions of the traits we all have
4.1.1. Personality becomes disorder when it causes problems for the person in terms of subjective distress or impairment
4.2. odd/eccentric personalities (includes schizotypal, which is characterized by odd thinking and behaviors)
4.3. >anxious or fearful personalities (includes dependent and avoidant personalities, associated with different types of social anxiety)
4.4. Dramatic or erratic behaviors
4.4.1. Borderline Personality Disorder
4.4.1.1. very volatile emotions, and some very dichotomous or black-and-white thinking= either great or terrible, friend or enemy, no in between. Not a lot of in-between or subtlety about their reactions to the world or to people.
4.4.1.2. Tend to have impulse control problems and tend to be selfish and appear manipulative
4.4.1.3. /High levels of neuroticism, low levels of conscientiousness agreeableness/
4.4.2. Antisocial Personality Disorder
4.4.2.1. /Low levels of conscientiousness and agreeableness, but unlike borderline has low levels of neuroticism
4.4.2.2. don’t tend to be afraid of much and they are calm in social situations where others might get nervous = might be because they don’t really have strong bonds with other people, and tend to not care how others view them
5. Defining disorders
5.1. statistically rare
5.2. biological dysfunction
5.2.1. not functioning properly
5.3. subjective distress
5.3.1. whether someone is suffering as a result of the symptom or trait
5.4. impairment
5.5. Must rule out alternatives
5.5.1. e.g.)medical causes of symptoms/side effects of prescribed meds
5.6. "abnormal" = need diagnosis for treatment
6. Anxiety Disorders
6.1. fear or worry that is out of control or out of proportion
6.1.1. major consideration is the subjective distress of the person with anxiety and the likelihood that anxiety will impair aspects of the person’s life
6.2. Generalized Anxiety Disorder (GAD) Always present. Isn’t tied to a particular trigger or situation
6.2.1. People tend to always be worried or on edge, but not about anything specific
6.3. Panic Disorder seem to come out of nowhere (although worrying about panic can bring on a panic attack) and is an extra large and unhelpful fight-or-flight reaction complete with high heart rate, sweating, trembling, shortness of breath, and a feeling like you’re about to die.
6.3.1. only diagnosed if you’ve had repeated panic attacks and it has affected your life negatively
6.4. Specific Phobias are tied to very specific triggers -fear has to be out of proportion to the risk, and it has to cause subjective distress or lead to some sort of impairment
6.4.1. e.g.) you have fear of dogs and you quit your job because your co-worker who is blind uses a service dog.
6.5. Social Anxiety Disorder is related to this category because the similar symptoms are similar -triggers are social situations where you might feel evaluated or judged
6.5.1. e.g.) job interview or public speaking, parties
6.6. Not technically anxiety disorders
6.6.1. Post-Traumatic Stress Disorder, or PTSD has a specific trigger that starts the disorder; anxiety is major component of symptoms
6.6.1.1. Traumatic event is defined= the person felt that their life was at risk or where they are exposed to the trauma of others.
6.6.2. Obsessive-Compulsive Disorder (OCD)-obsessions or compulsions must take up a significant amount of time or cause distress or impairment, and can’t be explained by some other disorder
6.6.2.1. Obsessions are intrusive thoughts or ideas that the person tries to suppress or get rid of.
6.6.2.2. Compulsions are mental acts or actions (like praying, counting, or hand washing) that are used to reduce anxiety (typically brought on by the obsessions).
6.7. genetic or heritable component to anxiety disorders, as well as obsessive compulsive disorders
6.7.1. strong heritable component to the personality trait of neuroticism
6.7.2. genes associated with the production and use of neurotransmitters like norepinephrine that are associated with alarm and fear reactions
6.7.3. people can learn to be afraid of specific stimuli, and that specific events can trigger the onset of symptoms
7. Diagnosis
7.1. DSM-5
7.1.1. Categorical approach = people are described as having a disorder or not and being diagnosed with a specific disorder within a specific category of disorders
7.1.2. Dimensional approach = people are rated along a spectrum for each symptom and their final ‘diagnosis’ would be a description of where they are at for each symptom
7.1.2.1. g.) similar to the Big Five model to describe personality.
7.1.3. Descriptive = under diagnostic criteria provide descriptions of the symptoms associated with each disorder other details about success rates for some treatments.
7.1.3.1. does not provide information about the causes of the disorder. This allows it to be used by a wide range of clinicians who may not all agree on those details
7.1.4. Diagnosis for a disorder includes checklists of symptoms, duration of symptoms, and other factors

