1. Free Fatty Acids (FFA)
1.1. What?
1.1.1. FFA are long chain carboxylic acids, that can be non-esterfied (NEFA), and are classified as lipids.
1.1.1.1. Under aerobic conditions FFA is a fuel for cardiac contractions. Yet under ischemic conditions FFA is dangerous.
1.1.1.1.1. Beta-oxidation (metabolism of FFA) produces toxic intermediates. These include catecholamine, which increases FFA release from adipose tissue and decreases insulin, which is responsible for taking up glucose into the myocardial cells.
1.1.1.1.2. Inhibits the oxidation of glucose
1.1.1.1.3. Leads to oxidation being uncoupled from the electron transport chain.
1.1.1.2. Image of a FFA.
1.2. How?
1.2.1. Triglycerols are hydrolyzed to from fatty acids, or fatty acids are synthesized from acetyl- or malonyl-CoA.
1.3. Why?
1.3.1. FFA are important components of a cell's membrane wall, and more importantly, it is a major energy source. It also serves as a potential danger.
1.3.1.1. More ATP and therefore oxygen is required to use FFA as a fuel, compared to glucose. This mean glucose is a more efficient fuel per oxygen molecule than FFA.
1.3.1.1.1. Activation of FFA requires energy, 2ATPs.
1.3.1.1.2. High FFA use may uncouple mitochondrial respiration.
1.3.1.2. Beta-oxidation of FFA produces a high amount of ATP, therefore it is a major fuel for energy production.
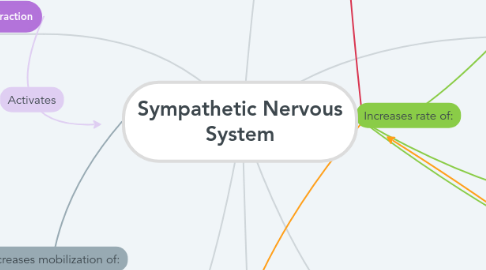
1.3.1.2.1. FFA mobilization is increased with sympathetic nervous activity. This situation may occur throughout anxiety or exercise.
2. Myocardial Infraction
2.1. What?
2.1.1. It is the reduction in blood flow through the coronary arteries, therefore reducing or blocking blood flow and consequently the amount of oxygen the heart receives.
2.2. How?
2.2.1. Due to the cardiac muscle not receiving enough blood and oxygen, the muscle cannot generate contraction as ATP is not available, and a heart attack occurs.
2.3. Why?
2.3.1. It occurs due to cholesterol partially or completely blocking the coronary arteries, as cholesterol plaques form against the vessel wall.
2.3.1.1. FFA is hydrolyzed from triglycerols, which is classified as a cholesterol.
3. Defined
3.1. What?
3.1.1. The subdivision of the autonomic nervous system that dominates in emergency or stressful situations, and prepares the body for strenuous physical activity.
3.2. How?
3.2.1. Consists of both presynaptic neurons and postsynaptic neurons. Presynaptic neurons release acetylcholine (ACh) which binds to nicotinic ACh, allowing postsynaptic fibers to be stimulated and release epinephrine or norepinephrine, which affects the target organs or tissues.
3.3. Why?
3.3.1. The sympathetic nervous system (SNS) is crucial in maintaining homeostasis and correcting imbalances in the body due to extrinsic factors.
4. Heart Rate
4.1. What?
4.1.1. The number of heart beats per unit of time, which is based on ventricular contraction.
4.2. How?
4.2.1. Auto-rhythmic cells display pacemaker activity, which causes depolarization and repolarization of the atria and ventricles. this electrical activity leads to the contractions of the atria and ventricles.
4.2.1.1. Electrical activity and rhythm is measured by a electrocardiogram (ECG)
4.3. Why?
4.3.1. Heart rate is an important factor in distribution of blood to the body. This factor can give important information of heart disease or abnormalities.
4.3.1.1. Bradycardia.
4.3.1.2. Tachycardia
5. Heart Contraction
5.1. What
5.1.1. The action of pumping blood to the rest of the body, by atria and ventricles contracting and relaxing.
5.2. How?
5.2.1. Auto-rhythmic cells create electrical activity, which causes contraction of the myocardial tissue in the heart.
5.2.1.1. Passive filling of the ventricular and atrial diastole.
5.2.1.1.1. End diastolic volume (EDV)
5.2.1.2. Atrial contraction occurs.
5.2.1.3. Isovolumetric ventricular contraction.
5.2.1.4. Ventricular ejection.
5.2.1.5. Isovolumetric ventricular relaxation.
5.2.1.6. Heart contractility can increase with a higher rate of influx of calcium ions, which is triggered by epinephrine and norepinephrine.
5.3. Why?
5.3.1. Disease and abnormalities
5.3.1.1. Atrial vibrilation.
5.3.1.2. Ventricular vibrilation.
5.3.1.3. Heart block.
6. Mean Arterial Pressure (Blood Pressure)
6.1. What?
6.1.1. The average pressure responsible for driving blood forward through the arteries into tissue, throughout the cardiac cycle.
6.1.1.1. BP = Cardiac Output x Total Peripheral Resistance
6.2. How?
6.2.1. Blood will flow down the pressure gradients, therefore from high pressure to low pressure throughout the body's vascular system.
6.2.1.1. Vasoconstriction
6.2.1.2. Vasodilation
6.2.1.3. Blood pressure is controlled by the cardiovascular-control center in the medulla, within the brain stem. Baroreceptors are responsible to sense changes in blood pressure, and send afferent impulses to the medulla.
6.2.1.3.1. The integration center alters the ratio of control between the parasympathetic and sympathetic system. Sympathetic nervous system is responsible for increasing vasoconstriction, which increases total peripheral resistance, and therefore results in increased blood pressure.
6.3. Why?
6.3.1. Blood pressure is an important factor is recognizing disease and abnormalities in the body.
6.3.1.1. Hypertension
6.3.1.2. Atrial Stiffness
