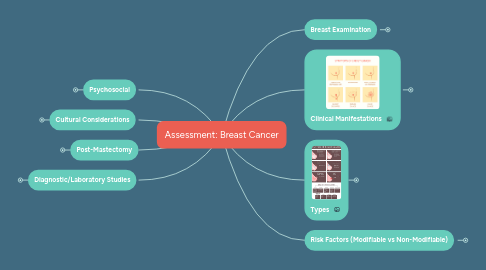
1. Psychosocial
1.1. Emotional wellbeing
1.2. Patient's needs for information
1.2.1. Advancement of disease
1.2.2. Treatment options
1.2.3. Side effects
1.3. Problems with sexuality
1.3.1. Sexual dysfunctions & body image
1.3.1.1. Threats to one's femininity
1.3.1.2. Loss of libido
1.3.1.3. Sexual relations with partners
1.4. Question
1.4.1. A patient who is scheduled for a lumpectomy and axillary lymph node dissection tells the nurse, "I would rather not know much about the surgery." Which response by the nurse is best?
1.4.1.1. "Tell me what you think is important to know about the surgery."
1.4.1.2. "It is essential that you know enough to provide informed consent."
1.4.1.3. "Many patients do better after surgery if they have more information."
1.4.1.4. "You can wait until after surgery for teaching about pain management."
2. Cultural Considerations
2.1. Some cultures do not allow the man to be part of the woman's care
2.1.1. Arab Muslim women
2.2. Male-predominant culture
2.2.1. All decisions about female care made by the man
2.2.1.1. Nigerian women
3. Post-Mastectomy
3.1. Post-op care
3.1.1. Vital signs
3.1.1.1. Q30 Mins x 2, Q1H x 2, then Q4H
3.1.1.2. Neuropathic pain
3.1.1.2.1. Inside of the armpit to the elbow
3.1.2. Dressings, drainage tubes & amount of drainage
3.1.2.1. Jackson Pratt
3.1.2.1.1. Drainage amount < 25 mL in 24-hour period
3.1.2.1.2. Remain in place 1 -3 Weeks
3.1.3. Arm and shoulder mobility
3.1.3.1. Adhesive capsulitis ("frozen shoulder")
3.1.4. Complications
3.1.4.1. Lymphadema
3.1.4.2. Bleeding
3.1.4.3. Infection
3.1.4.4. Lack of perfusion
4. Diagnostic/Laboratory Studies
4.1. Imaging studies
4.1.1. Mammography
4.1.1.1. Gold standard
4.1.2. Ultrasound
4.1.2.1. Rarely use
4.1.2.1.1. Use In addition to mammography
4.1.2.1.2. Mostly for dense breast
4.1.2.2. Differentiating fluid-filled cysts vs solid mass
4.1.3. MRI
4.1.3.1. Only for high-risk women
4.2. Breast biopsy
4.2.1. Definitive diagnosis
4.3. Pathologic studies of lymph nodes
4.3.1. Metastasis
4.4. Liver Enzymes
4.4.1. Liver metastasis
4.5. Serum calcium and alkaline phosphatase
4.5.1. Bone Metastasis
5. Breast Examination
5.1. Assessing breast mass
5.1.1. Location of the mass
5.1.1.1. "Face of the clock" method
5.1.2. Describe shape, size and consistency
5.1.3. Is the mass fixed or movable?
5.1.4. Note skin changes around the mass
5.1.4.1. Dimpling?
5.1.4.2. Peau d'Orange?
5.1.4.3. Nipple retraction?
5.1.4.4. Discharge?
5.1.5. Assess adjacent lymph nodes
5.1.5.1. Axillary
5.1.5.2. Supraclavicular
5.1.6. Ask about pain or soreness in the area of the mass
6. Clinical Manifestations
6.1. Breast lumps
6.1.1. Hard, fixed and irregular
6.1.1.1. Often in upper outer breast quadrant
6.1.2. Movable and round or oval
6.1.2.1. Most likely benign
6.2. Nipple Discharge
6.2.1. unilateral
6.2.1.1. bloody or non-bloody
6.3. Dimpling or skin retraction
6.3.1. Retraction of breast ligament
6.4. Eczema-like rash on breast
6.4.1. Paget disease
6.5. Ulceration
6.5.1. Tumor necrosis
6.6. Breast edema
6.6.1. Peau d'Orange
6.7. Metastatic Breast CA
6.7.1. Bone pain
6.7.2. Pleural effusion
6.7.2.1. Metastasis to pleural cavity
6.7.2.2. SOB
6.7.3. Chest pain
6.7.3.1. Metastasis to thoracic cavity
6.7.4. Edema of the arm
6.7.4.1. Obstruction of lymphatic in the axilla
6.7.5. Neuropathic pain
6.7.5.1. May radiate to chest, back, scapula
6.7.6. Headache or seizure
6.7.6.1. Brain metastasis
7. Types
7.1. Non-invasive breast CA = 20%
7.2. Invasive breast CA = 80%
7.3. Common sites of breast CA metastasis
8. Risk Factors (Modifiable vs Non-Modifiable)
8.1. High increased risk
8.1.1. Female
8.1.2. Age > 65
8.1.3. Genetics
8.1.3.1. BRCA 1 and BRCA 2
8.1.4. History of previous breast CA
8.1.5. Breast density
8.1.5.1. More glandular and connective tissues
8.1.6. Atypical hyperplasia
8.2. Moderate increased Risk
8.2.1. Family history
8.2.2. Ionizing radiation
8.2.2.1. Frequent exposure
8.2.3. High postmenopausal bone density
8.2.3.1. High estrogen levels
8.3. Low increased risk
8.3.1. Nullparity or first child born after age 30 years
8.3.2. Early menarche or late menopausal
8.3.3. Recent oral contraceptives or hormonal replacement therapy (HRT) use
8.3.4. Obesity
8.3.4.1. Postmenopausal obesity
8.3.5. ETOH
8.4. Cultural Considerations
8.4.1. African-American, Hawaiian, Puerto Rican, and Samoan women
8.4.1.1. Highest risk of breast CA
8.5. Question
8.5.1. The nurse is caring for four clients. Which client does the nurse recognize as having the highest risk for development of breast cancer?
8.5.1.1. a. 45-year-old male with gynecomastia
8.5.1.2. b. 40-year-old female whose father had colon cancer
8.5.1.3. c. 50-year-old male whose mother had ovarian cancer
8.5.1.4. d. 65-year-old female with history of a prior episode of breast cancer
