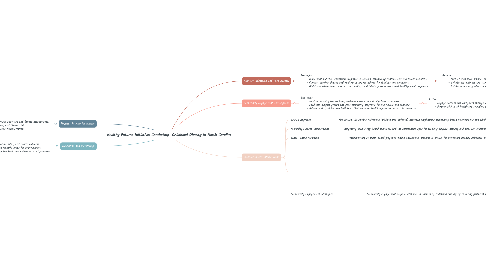
1. Physical Activity Promotion:
1.1. Strategies: - Enhance physical education curriculum with age-appropriate activities and fitness assessments. - Organize after-school sports leagues, intramural programs, and fitness clubs. - Implement walking and biking initiatives to promote active transportation.
1.1.1. Actions: - Work with schools to improve playgrounds, gymnasiums, and outdoor recreation spaces. - Partner with local sports organizations to provide coaching and equipment. - Advocate for safe walking and biking routes in the community.
1.1.1.1. Stakeholders: - School administrators, physical education teachers, and coaches. - Local sports clubs, recreation centers, and parks departments. - Transportation planners, city councils, and community activists.
2. Evaluation and Monitoring:
2.1. - Strategies: - Establish a system for collecting data on program implementation, participation rates, and health outcomes. - Conduct regular evaluations to assess the effectiveness of interventions and identify areas for improvement. - Use data-driven insights to adapt and refine strategies based on community feedback and evidence-based practices.
2.1.1. - Actions: - Develop evaluation tools, surveys, and assessment protocols to measure program impact and outcomes. - Collaborate with research institutions and academic partners to conduct longitudinal studies and program evaluations. - Engage community members in the evaluation process through focus groups, feedback sessions, and advisory boards.
2.1.1.1. - Stakeholders: - Program managers, data analysts, and research coordinators. - Community members, program participants, and key stakeholders. - Funding agencies, grantmakers, and philanthropic organizations.
3. Nutrition Education and Food Access:
3.1. Strategies: - Implement nutrition education programs in schools, community centers, and healthcare facilities. - Conduct cooking classes and healthy eating workshops for families and caregivers. - Distribute educational materials on reading food labels, portion sizes, and healthy meal preparation.
3.1.1. Actions: - Partner with local schools to integrate nutrition education into the curriculum. - Collaborate with grocery stores to promote healthy food options and offer discounts on fresh produce. - Establish school gardens or community farms to provide hands-on learning opportunities.
3.1.1.1. Stakeholders: - School administrators, teachers, and nutrition staff. - Local farmers, grocery store owners, and food suppliers. - Healthcare providers, dietitians, and nutritionists.
4. Community Engagement and Support:
4.1. Strategies: - Host community health fairs, wellness events, and family fitness activities. - Facilitate support groups and peer mentoring programs for individuals and families. - Advocate for policies and initiatives that promote health equity and access to resources.
4.1.1. Actions: - Engage parents and caregivers through outreach events, workshops, and social media campaigns. - Partner with local healthcare providers to offer screenings, counseling, and referrals. - Collaborate with community organizations to address social determinants of health such as poverty and food insecurity.
4.1.1.1. Stakeholders: - Community leaders, social workers, and public health professionals. - Local businesses, faith-based organizations, and civic groups. - Policy makers, advocacy organizations, and government agencies.
