Cerebral Vascular Accident (CVA)
por Stephanie Carr
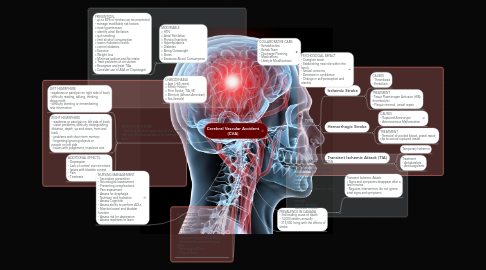
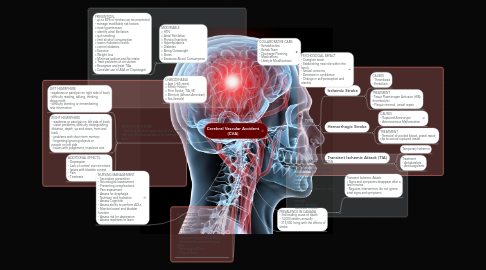
1. RISK FACTORS
1.1. MODIFIABLE » HTN » Atrial Fibrilation » Physical Inactivity » Hyperlipidemia » Diabetes » Being Overweight » Stress » Excessive Alcool Consumption
1.1.1. PREVENTION - up to 80% of strokes can be prevented - manage modifiable risk factors: » treat hypertension » identify atrial fibrilation » quit smoking » limit alcohol consumption » lower cholesterol levels » control diabetes » Exercise » Weight loss » Minimize sodium and fat intake » Treat problems of circulation » Recognize and treat TIAs » Consider use of ASA or Clopidogrel
1.2. UNMODIFIABLE » Age (>65 years) » Family History » Prior Stroke, TIA, MI » Ethnicity (African American) » Sex (female)
2. DIAGNOSTICS - Angiography / Arteriography - Blood and Urine Tests - Carotid Doppler - CT Scan - Echocardiogram - Electrocardiogram (ECG/EKG) - Magnetic Resonance Imaging (MRI) - Neurological Exam - Physical Exam
3. EFFECTS OF STROKE: - Recovery depends upon area of the brain that was affected and size of the damaged area
3.1. LEFT HEMISPHERE - weakness or paralysis on right side of body - difficulty reading, talking, thinking, doing math - difficulty learning or remembering new information
3.2. RIGHT HEMISPHERE - weakness or paralysis on left side of body - vision problems; difficulty distinguishing distance, depth, up and down, front and back - problems with short-term memory - forgetting/ignoring objects or people on left side - issues with judgement, impulsive acts
3.3. ADDITIONAL EFFECTS: - Depression - Lack of control over emotions - Issues with bladder control - Pain - Tiredness
4. NURSING MANAGEMENT - Secondary prevention - Neurological assessment - Preventing complications - Pain assessment - Assess for dysphagia - Nutrition and hydration - Assess Cognition - Assess ability to perform ADLs - Monitor bowel and bladder function - Assess risk for depression - Assess readiness to learn
5. PREVALENCE IN CANADA - 3rd leading cause of death - 14,000 deaths annually - 315,000 living with the effects of stroke
6. TYPES
6.1. Ischemic Stroke
6.1.1. CAUSES - Thrombosis - Embolism
6.1.2. TREATMENT -Tissue Plasminogen Activator (tPA): thrombolytic - Plaque removal, vessel repair
6.2. Hemorrhagic Stroke
6.2.1. CAUSES - Ruptured Anneurysm - Arteriovenous Malformation
6.2.2. TREATMENT - Removal of pooled blood, vessel repair, clip to secure ruptured vessel
6.3. Transient Ischemic Attack (TIA)
6.3.1. Temporary Ischemia
6.3.2. Treatment - Antiplatelets - Anticoagulants
