1. PCOR Engagement Principles
1.1. Reciprocal Relationships:
1.1.1. Describe the roles and decision-making authority of all research partners, including patient and stakeholder partners.
1.1.2. Examples of how to demonstrate this in your proposal:
1.1.2.1. Explain how decision-making is made within your research team, including the decision-making authority that patient and stakeholder partners have and in what circumstances.
1.1.2.2. Include patient and stakeholder partners as key personnel, with biosketches illustrating how the skills and experiences of the patient partners prepare them to function effectively in this role.
1.2. Co-learning:
1.2.1. Describe plans to ensure that patient and stakeholder partners will understand the research process and researchers will understand patient and stakeholder engagement and patient-centeredness.
1.2.2. Examples of how to demonstrate this in your proposal:
1.2.2.1. Training and educational opportunities are provided, such as patient and stakeholder partner training in human subjects protection.
1.2.2.2. Training is provided by patient advocacy organizations, patients/survivors, and clinicians/ caregivers for the researchers providing the intervention (e.g., training in better communication with patients,led by patient instructors).
1.3. Partnership:
1.3.1. Describe how the time and contributions of patient partners are valued and demonstrated in fair financial compensation, as well as reasonable and thoughtful time commitment requests.
1.3.2. Examples of how to demonstrate this in your proposal:
1.3.2.1. Compensation for patient partners is included in the budget at an appropriate level.
1.3.2.2. Meetings are held at a time and in a location that accommodates patient and stakeholder partners. Compensation is provided for transportation and related expenses.
1.3.2.3. Accommodations are made to encourage the full engagement of a diversity of patient and stakeholder partners, and the research team includes a diversity of members. For example, a project that focuses on Latino health should consider including Spanish-speaking individuals on the research team and may wish to conduct patient and stakeholder meetings in both Spanish andEnglish.
1.4. Trust, Transparency, Honesty:
1.4.1. Describe how major decisions are made inclusively and information is shared readily with all research partners, including patient and stakeholder partners; patient and stakeholder partners and research partners express commitment to open and honest communication with one another; and the study team commits to communicate study findings to the community studied, in a meaningful and usable way.
1.4.2. Examples of how to demonstrate this in your proposal:
1.4.2.1. Commitments to trust, transparency, and honesty are stated in many applications. These commitments can be demonstrated through describing how the research team—including patient and stakeholder partners—will communicate with each other, the frequency of this communication, the roles of each member of the research team, and the decision-making authority of each member of the research team.
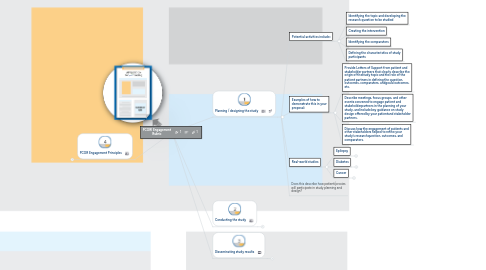
2. Planning / designing the study
2.1. Potential activities include:
2.1.1. Identifying the topic and developing the research question to be studied
2.1.2. Creating the intervention
2.1.3. Identifying the comparators
2.1.4. Defining the characteristics of study participants
2.2. Examples of how to demonstrate this in your proposal:
2.2.1. Provide Letters of Support from patient and stakeholder partners that clearly describe the origin of thestudy topic and the role of the patient partners in defining the question, outcomes, comparators, andgoals/outcomes, etc.
2.2.2. Describe meetings, focus groups, and other events convened to engage patient and stakeholderpartners in the planning of your study, and include key guidance on study design offered by your patientand stakeholder partners.
2.2.3. Discuss how the engagement of patients and other stakeholders helped to refine your study’s researchquestion, outcomes, and comparators.
2.3. Real-world studies
2.3.1. Epilepsy
2.3.1.1. The patients and parents of patients with epilepsy pose the question: Which anti-epileptic drugs best preserve sufficient cognition to go to work or school and to function normally, while still preventing seizures adequately?
2.3.2. Diabetes
2.3.2.1. Clinicians who reviewed the initial study design indicated that clinical practice is quite variable and suggested that a three-arm approach would be more appropriate for the study. The study design was revised accordingly.
2.3.3. Cancer
2.3.3.1. Patient partners determine that all women with breast cancer would be eligible versus only women who had completed active treatment.
2.4. Does this describe how patient/proxies will participate in study planning and design?
3. Conducting the study
3.1. Potential activities include:
3.1.1. Participating in and monitoring the conduct of the project
3.1.2. Assisting with the recruitment of study participants
3.1.3. Assisting with data collection and data analysis
3.1.4. Participating in the evaluation of patient and stakeholder engagement
3.2. Examples of how to demonstrate this in your proposal:
3.2.1. Provide Letters of Support from patient and stakeholder partners that clearly describe the role of thesepartners in conducting and monitoring the study.
3.2.2. Clearly articulate in the application the roles of the patient and stakeholders partners in eachcomponent of study conduct (e.g., helping to draft survey tools and focus group questions, reviewingparticipant materials for readability, etc.), including the dissemination and implementation assessment.
3.2.3. Include a plan for “check-ins” with patient and stakeholder partners to monitor their perceptions of the extent to which (a) they are meaningfully involved in the study and (b) their participation is contributing to the study. Plan similar “check-ins” with other research team members to monitor and evaluate engagement in the project.
3.3. Real-world studies
3.3.1. Chronic pain
3.3.1.1. The informed consent document is developed with patient partners to make itunderstandable to study participants.
3.3.2. Depression
3.3.2.1. Patient advocacy groups assist with recruitment through their patient networks—the“book club” model.
3.3.3. Preeclampsia
3.3.3.1. Study team will recruit via a national network of local health departments and community health centers, as well as a preeclampsia advocacy group’s website, and Facebook page.
4. Disseminating study results
4.1. Potential activities include:
4.1.1. Identifying partner organizations for dissemination
4.1.2. Planning dissemination efforts
4.1.3. Participating in dissemination efforts, such as the authoring of manuscripts and the presentation ofstudy findings
4.2. Examples of how to demonstrate this in your proposal:
4.2.1. Clearly identify the role of patient and stakeholder partners in planning the dissemination of the study’sfindings.
4.2.2. Include patient and stakeholder partners on project committee that will oversee dissemination.
4.2.3. Include patient and stakeholder partners in dissemination and implementation assessment.
4.3. Real-world studies
4.3.1. Trauma
4.3.1.1. The research team will convene a policy summit with relevant professional societies during the third year of the study to focus on identifying ways to speed the implementation of findings into practice.
4.3.2. Cardiac
4.3.2.1. A Patient Dissemination Board is helping to craft the dissemination plan and advise the research team on how to best share study findings.
4.3.3. Chronic pain
4.3.3.1. Patient partners co-author manuscripts, present at scientific and lay conferences, and share study findings through their networks.
