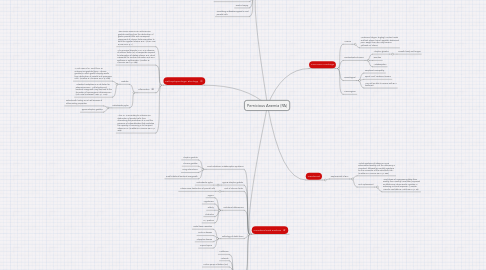
1. Pathophysiologic Etiology
1.1. "Pernicious anemia is an autoimmune gastritis resulting from the destruction of gastric parietal cells and consequent impairment of intrinsic factors secretion to bind the ingested vitamin B12" (Chan, Low & Lee 2016, p. 1)
1.2. "The principal disorder in PA is an absence of intrinsic factor (IF), a transporter required for absorption of dietary vitamin B12, which is essential for nuclear maturation and DNA synthesis in erythrocytes" (Huether & McCance 2014, p. 988).
1.3. Inflammation
1.3.1. Gastritis
1.3.1.1. "Most cases of PA result from an autoimmune gastritis (type A chronic gastritis) in which gastric atrophy results from destruction of parietal and zymogenic cells" (Huether & McCance 2014, p. 988).
1.3.1.2. "Intestinal metaplasia is a risk factor for adenocarcinoma. Achlorhydria and bacterial overgrowth may also lead to the formation of carcinogenic nitrosoamines" (Toh, Direl & Gleeson 1997, p. 1446).
1.3.2. Helicobacter pylori
1.3.2.1. Patients with history are at risk because of inflammatory properties
1.3.2.2. Type B atrophic gastritis
1.4. "This, PA is secondary to autoimmune destruction of parietal cells, thus diminishing the production of IF, and the presence of autoantibodies that neutralize the capacity of remaining IF to transport vitamin B12" (Huether & McCance 2014, p. 988).
2. Causitive/Risk Factors
2.1. Food-cobalamin malabsorption syndrome
2.1.1. Atrophic gastritis
2.1.2. Chronic gastritis
2.1.3. Drug interactions
2.1.4. Small intestinal bacterial overgrowth
2.2. Type B atrophic gastritis
2.2.1. Helicobacter pylori
2.3. Lack of intrinsic factor
2.3.1. Autoimmune destruction of parietal cells
2.4. Nutritional deficiencies
2.4.1. Vegans
2.4.2. Vegetarians
2.4.3. Elderly
2.4.4. Alcoholics
2.4.5. HIV positive
2.5. Pathology of distal ileum
2.5.1. Distal ileum resection
2.5.2. Crohn's disease
2.5.3. Whipple's disease
2.5.4. Tropical sprue
2.6. Drugs
2.6.1. Metformin
2.6.2. Antacids
2.6.3. Proton pump inhibitors (PPI)
2.6.4. H2 blockers
2.6.5. Colchicine
2.6.6. Phenytoin
2.6.7. Zidovudine
2.7. Imerslund-Grasbeck syndrome, surgical gastrectomy, intestinal parasites, nitrous oxide inhalation, infants of mother's with the condition
3. Diagnostic Tests
3.1. "Although many clinical laboratories define B12 deficiency at a level of <150 pg/ml (<110 pool/ L; pool/L + pg/ml X 0.738), or in some cases <200 pg/ ml (<148 pool/L), patients with values above these levels may be symptomatic and benefit from treatment" (Manolis, Manolis, Poulidakis & Melita 2013, p. 54).
3.2. Schilling test (outdated)
3.3. Methylmalonic acid and homocysteine levels
3.4. Gastric biopsy
3.5. Circulating antibodies against IF and parietal cells
4. Common Findings
4.1. Anemia
4.1.1. Weakness, fatigue, tingling/ number hands and feet, ataxia, loss of appetite, abdominal pain, weight loss, skin may become yellowish w/ icterus
4.2. Gastrointestinal issues
4.2.1. Atrophic glossitis
4.2.1.1. Smooth beefy red tongue
4.2.2. Diarrhea
4.2.3. Malabsorption
4.3. Neurological
4.3.1. Peripheral neuropathy
4.3.2. Spinal cord/ cerebrum lesions
4.3.3. May not be able to reverse with B12 treatment
4.4. Carcinogenic
5. Treatment
5.1. Replacement of B12
5.1.1. "Initial injections of vitamin B12 are administered weekly until the deficiency is corrected, followed by monthly injections for the remainder of the individual's life" (Huether & McCance 2014, p. 988).
5.1.2. Oral replacement
5.1.2.1. "Oral doses of 1000-2000 ug/day, then weekly, then monthly have been proposed as effective as intramuscular injection in achieving a clinical response" (Manolis, Manolis, Poulidakis & Melita 2013, p. 55).
