1. Introduction
1.1. Normocytic-Normochromic Anemias
1.1.1. Are less frequent than macrocytic-normochromic and microcytic-hypochromic anemias.
1.1.2. No common cause, pathologic mechanisms, or morphologic characteristics exist.
1.2. Other types of Normocytic-Normochromic Anemias besides Aplastic Anemia
1.2.1. Post-hemorrhagic anemia
1.2.2. Anemia of chronic disease
1.3. Aplastic Anemia
1.3.1. Pancytopenia
1.3.1.1. Reduction or absence of all 3 types of blood cells
1.3.2. Pure RBC aplasia
1.3.2.1. Only RBCs are affected
1.3.3. Fanconi anemia
1.3.3.1. Rare genetic anemia from defects in DNA repair
2. Pathophysiologic Etiology
2.1. Hypocellular bone marrow that has been replaced with fat
2.2. Clinical Manifestations
2.2.1. Hypoxemia, pallor (occasionally with a brownish pigmentation of the skin)
2.2.2. Weakness along with fever and dyspnea with rapidly developing signs of hemorrhaging if platelets are affected
2.3. Diagnostic Tests and Evaluation
2.3.1. Bone Marrow Biopsy
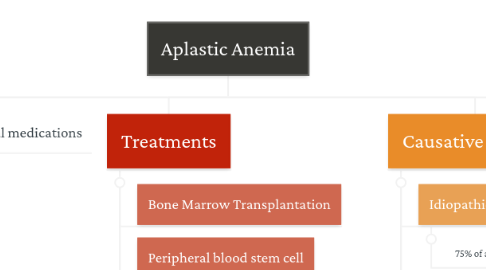
3. Corticosteroidal medications
4. Treatments
4.1. Bone Marrow Transplantation
4.2. Peripheral blood stem cell transplantation
4.2.1. May receive radiation or chemotherapy before procedure
4.3. Immunosuppression
4.3.1. Antithymocyte globulin with cyclosporin
4.4. If not treated or identified, death occurs
4.5. Identification of high-risk individuals
5. Causative Factors
5.1. Idiopathic
5.1.1. 75% of all confirmed cases
5.2. Secondary
5.2.1. 15% of cases
5.2.2. Caused by a variety of known chemical agents and ionizing radiation
5.2.2.1. Chemotherapeutic drugs, benzene, arsenic, and multiple drugs
5.2.2.1.1. Liver Disease (seronegative hepatitis)
5.3. Infection - specifically viruses: HIV, EBV, Hepatitis
5.3.1. Parvovirus B19
5.4. Total body irradiations
6. Risk Factors
6.1. Acquired rather than constitutional or hereditary
6.1.1. Some genetic risk factors
7. Common Findings
7.1. Relationship with Immunity
7.1.1. Individuals unable to undergo bone marrow transplantation or lack a suitable sibling donor: Immunosuppression is the treatment of choice
7.1.2. Recombinant hematopoietic growth factors, such as granulocyte-macrophage colony-stimulating factor (GM-CSF)
7.1.2.1. IL-6 and epoetin are also significant additional benefit
7.2. Immunosuppression is not without risk
7.2.1. Individuals receiving immunosuppressive therapy are at risk of experiencing treatment failure or late clonal/malignant conditions, or both.
7.2.2. Late clonal/malignant conditions include paroxysmal nocturnal hemoglobinuria (PNH), MDS, acute leukemia, or solid tumor.
7.2.2.1. Although quite rare (less than 3%) administration of ATG may cause an anaphylactic reaction in some individuals.

