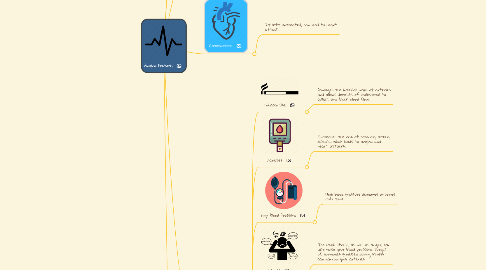
1. Definition
1.1. A term used for chest pain caused by reduced blood flow to the heart muscle.
2. Other Types of Angina
2.1. Unstable Angina
2.1.1. Reduced blood flow to the heart muscle because the coronary arteries are narrowed by fatty build-ups.
2.1.1.1. Symptoms often occur while you may be resting, sleeping, or using little physical exertion. This type of angina usually comes as a surprise and can last longer than stable angina and could lead to a heart attack.
2.2. Microvascular Angina
2.2.1. Spasms within the walls of the small arterial blood vessels causes reduced blood flow to the heart muscle.
2.2.1.1. Symptoms are first noticed during daily activities or times of stress. Often occur with shortness of breath, sleep problems, fatigue, and lack of energy. The pain/discomfort is often more severe than other types of angina.
2.3. Prinzmetal Angina
2.3.1. Caused by spasms in the coronary arteries.
2.3.1.1. Symptoms occur when the pain or discomfort usually occurs while resting and during the night or early morning hours. The pain/discomfort is usually severe.
3. Treatment Options
3.1. Rest
3.1.1. Relaxing allows the coronary arteries to increase the heart's blood supply.
3.2. Nitroglycerin
3.2.1. Relaxes the coronary arteries and other blood vessels, reducing the amount of blood that returns to the heart and easing the heart's workload.
4. Complications
4.1. If left untreated, can lead to heart attack.
5. Symptoms
5.1. The pain or discomfort often occurs when the heart must work harder, like during physical activity. These episodes do not typically come as a surprise. They may feel like: gas, indigestion or chest pain that spreads to the arms, back, or other areas.
6. Risk Factors
6.1. Tobacco Use
6.1.1. Damages the interior walls of arteries and allows deposits of cholesterol to collect and block blood flow.
6.2. Diabetes
6.2.1. Increases the risk of coronary artery disease, which leads to angina and heart attacks.
6.3. High Blood Pressure
6.3.1. High blood pressure damages arteries over time.
6.4. Stress
6.4.1. Too much stress, as well as anger, can also raise your blood pressure. Surges of hormones produced during stress can narrow your arteries.
6.5. Old age
6.5.1. Men older than 45 and women older than 55 have a greater risk than do younger adults.
6.6. High blood cholesterol or triglyceride levels
6.6.1. Cholesterol can narrow arteries throughout your body, including those that supply your heart. High levels of the wrong kind of cholesterol, known as LDLs, increases your risk of angina. A high level of triglycerides, also increases your risk.
6.7. History of Heart Disease
6.7.1. If you have coronary artery disease or if you've had a heart attack, you're at a greater risk of developing angina pectoris.
6.8. Lack of Exercise
6.8.1. Inactive lifestyle contributes to high cholesterol, high blood pressure, type 2 diabetes and obesity
6.9. Obesity
6.9.1. Raises the risk of angina and heart disease because it's associated with high blood cholesterol levels, high blood pressure and diabetes.
