1. Tests
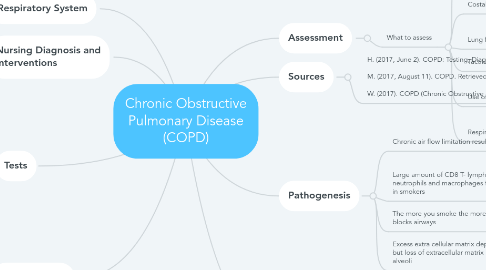
1.1. Chest X-ray
1.1.1. Can help rule out other conditions with similar symptoms such as lung cancer
1.1.2. Can show chronic lung conditions and complications related to these conditions
1.1.3. Can show changes or problems in lungs that stem from heart problems
1.2. Electrocardiogram
1.2.1. May find certain heart problems that can cause shortness of breath
1.3. Complete blood count
1.3.1. Measures cells that compose blood; person with COPD would show increased red and white blood cells
1.4. Arterial blood gases
1.4.1. Patients with COPD snow hypoxemia without hypercapnia
1.4.2. Measures how much oxygen and carbon dioxide is in the blood
1.4.3. Helps determine whether a patient needs oxygen treatment
2. Nursing Diagnosis and Interventions
2.1. Disturbed sleep pattern related to excessive coughing due to patient reporting increased coughing during the night and when they lay down.
2.1.1. Encourage patient to sleep in a chair so they do not cough as much since they will be sitting. Encourage the patient to sleep with two pillows th
2.2. Anxiety related to dyspnea and fear of suffocation as evidenced by patient reporting difficulty of breathing and shortness of breath.
2.2.1. Encourage patient to relax and take deep breaths. Educate patient on ways to relax and decrease stress like yoga and massages.
2.3. Impaired gas exchange related to chronic lung tissue damage secondary to chronic smoking as evidenced by patient reporting they smoke.
2.3.1. Encourage patient to stop smoking and suggest trying ways to cut down how much they smoke like trying nicotine gum and such.
2.4. Risk for activity intolerance related to imbalance between oxygen supply and demand
2.4.1. Encourage patient to rest and exercise a little bit a time. The patient can keep slowly increasing their activity until they are not in pain or discomfort while exercising.
3. Complications
3.1. Lung damage
3.2. Osteoporosis
3.3. Heart failure
3.3.1. Excess strain from pulmonary hypertension on the right ventricle
3.4. Collapsed lung
3.5. Sleep problems
3.5.1. Due to not being able to breath at night while laying down
3.6. Pneumonia
4. Respiratory System
4.1. Activity exercise pattern
5. Assessment
5.1. What to assess
5.1.1. Pulse oximetry
5.1.1.1. Place pulse oximeter on one finger of the patient and I️t will measure the blood oxygen saturation level. This should be between 94-99%.
5.1.2. Costal angle
5.1.2.1. Have patient breath in and place hands below the twelve rib and measure the space in between nurse’s thumbs.
5.1.3. Lung fields
5.1.4. Tactile fremitus
5.1.4.1. Have patient say “99”
5.1.5. Use of accessory muscles
5.1.5.1. Determine if patient uses sternocleidomastoid, pectoralis major or minor, the latissimus dorsi muscles etc. to assist with breathing
5.1.6. Respirations
5.1.6.1. Watch patient breath for one minute and record number
6. Pathogenesis
6.1. Chronic air flow limitation results from abnormal inflammatory responses to inhaled particles
6.1.1. Such as
6.1.1.1. Smoking cigarettes
6.1.1.2. Pollution
6.2. Large amount of CD8 T- lymphocytes neutrophils and macrophages found in smokers
6.3. The more you smoke the more it blocks airways
6.4. Excess extra cellular matrix deposition but loss of extracellular matrix in the alveoli
7. Causes
7.1. Smoking
7.1.1. Inhaled particles
7.2. Premature births that lead to lung damage
7.3. Exposure to lung irritants like chemicals, fumes, and industrial dust
7.3.1. Can be impacted by workplace, environment, pollution
7.4. Inherited genes
7.4.1. Such as
7.4.1.1. The IREB2 gene

