1. Associated Disease
1.1. Hyperthyroid, PE, Infection/Sepsis/Inflammation, drugs (cocaine)/alcohol
1.2. CAD, Rheumatic HD, HTN, Valvular HD, Hypertrophic cardiomyopathy
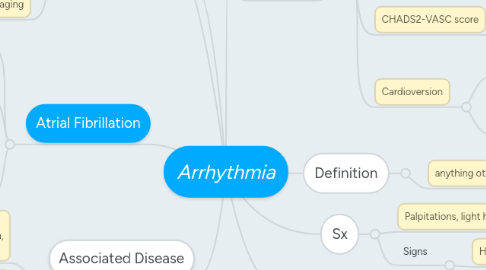
2. Atrial Fibrillation
2.1. Epidemiology
2.1.1. incidence: 5 mil/year, M>F, >age
2.2. Definition
2.2.1. Irregularly Irregular RR intervals, Narrow QRS complex, No distinct P waves
2.3. Types
2.3.1. Paroxsymal
2.3.1.1. <7 days w/ or w/o Rx, recur
2.3.2. Persistent
2.3.2.1. >7 days usually need Rx
2.3.3. Long-Standing
2.3.3.1. >1 YEAR
2.3.4. Permenant
2.3.4.1. Refractory
3. DDx: Atrial Flutter (sawtooth), WPW, ectopic PVC/PAC, MAT, sinus arrythmia
4. Investigations
4.1. ECG
4.1.1. 24 hr, event (30 days), implantable, stress test
4.2. Bloods
4.2.1. FBC, U/E, ESR/CRP, Troponin, BNP, TFT, tox screen, septic screen, glucose
4.3. Imaging
4.3.1. CXR, Echo, Cor angio
5. Definition
5.1. anything other then NSR
6. Sx
6.1. Palpitations, light headedness, awareness of HR, dizzy, chest pain, SOB, fatigue, pre-syncope
6.2. Signs
6.2.1. HTN, pulse, change in BP readings
7. Management
7.1. ECG, TE risk, Rate/Rhythm, CV disease risk
7.1.1. Rate control @ 80-100 bpm: BB or CCB
7.1.1.1. Stable
7.1.1.1.1. ORAL
7.1.1.2. Unstable
7.1.1.2.1. IV
7.2. CHADS2-VASC score
7.2.1. CCF/LVD, HTN, Age, DM, Stroke/TIA, Sex F, Vascular disease (stroke and age = 2)
7.2.1.1. >2 = oral anticoagulant
7.3. Cardioversion
7.3.1. When: shock, rate controlled but symptomatic, MI
7.3.2. How: if >48 hrs after AF onset, 3 week OAC then cardioversion OR <48hrs heparin, cardiovert THEN on stroke risk long term OAC after (except if <48hr onset + no RFs)
