1. Registration
1.1. Identification
1.1.1. Hospital and Department protocol
1.2. Payment
1.2.1. Cost
1.2.1.1. Subsidized
1.3. Instructions
1.3.1. Informed Consent
1.3.1.1. Not robust enough, High volume and time pressure, we may inject radioisotope by mistake
2. Imaging System QC
2.1. Calibration
2.2. Engineer Service
3. Interpretation
3.1. Image Quality
3.1.1. Experience and On the Job training with vendor
3.1.1.1. Can we use different parameter to improve image quality? A inter-institution and vendor collaboration will help
3.1.2. Optimal Diagnostic
3.2. Data
4. Patient Condition
4.1. Based on Experience/On the job training/ Department protocol
4.1.1. Unstable
4.1.1.1. To do last : Do the stable ones first. ( On the job training and Experienced Senior )
4.1.1.1.1. Do we have enough resources and manpower? We are depriving critically ill patients to do first
4.1.2. Stable
4.1.2.1. Usually, no issues however, patient may come unprepared due to poor communication
5. Too busy, and too many cases for a day, a brochure explaining after care
5.1. Is this enough?
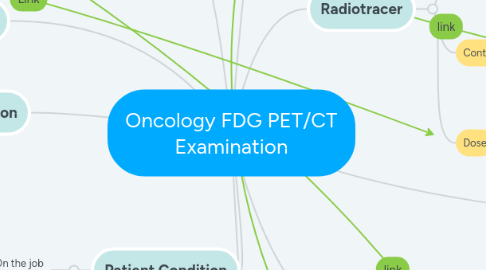
6. Radiotracer
6.1. Indications
6.1.1. Delbeke, Dominique, et al. (2006) SNMMI Guidelines "Procedure guideline for tumor imaging with 18F-FDG PET/CT 1.0"
6.1.1.1. In accordance to STANDARDS FOR THE PROVISION OF NUCLEAR MEDICINE, IMAGING, THERAPY AND ASSAY SERVICES Directed By Ministry of Health
6.1.1.2. Discussion with team of nurses, doctors and technologist is essential - to update protocol so that it is current and tailor to the patient individual needs
6.2. Contraindication
6.2.1. Pregnancy
6.2.1.1. Evidence, International Guideline and Protocol
6.2.1.1.1. Guidelines from CEA, F. A. R. (2001) and Wall, B. F. (2009) : The guidelines was revised recently to account high and lower dose for 14 -day rule and 28 day rule
6.3. Dose
6.3.1. Injection wrong dose on wrong patient
6.3.1.1. Systematic Error
6.3.1.1.1. Ensure to follow Directives provided by Ministry of Health
7. Post Imaging Care
7.1. Follow up
7.2. Instructions: From Senior Nurses
7.2.1. Poor Communication : Have we instruct patient well?
8. Communication
8.1. Language
8.1.1. Often experienced patients with a lot of anxiety
8.1.1.1. Acuff, S. N., Bradley, Y. C., Barlow, P., & Osborne, D. R. (2014). Reduction of patient anxiety in PET/CT imaging by improving communication between patient and technologist : suggest using a call device with regular check with patient to alleviate anxiety
8.2. Disability
8.2.1. Realized that we do not have skill staff to communicate with patient communicating disability, Thus training staff is imperative for proper informed consent.
8.2.1.1. Semelka, R. C., Armao, D. M., Elias Jr, J., & Picano, E. (2012). The information imperative: is it time for an informed consent process explaining the risks of medical radiation?. Radiology, 262(1), 15-18.
9. Technologist Competency
9.1. Education/ Experience
9.1.1. Is the curriculum promoting evidence based? Does this curriculum empower new technologist to take appropriate clinical decision when they encounter difficult situation with patients?
9.1.1.1. Medical Radiation Practice Board of Australia. (2020). Professional capabilities for medical radiation practice.
