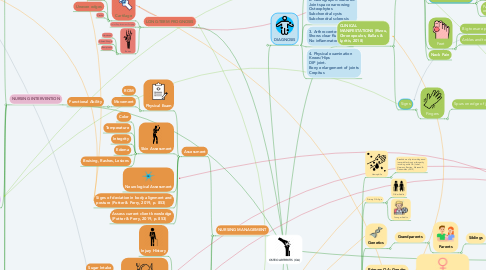
1. PATHOPHYSIOLOGY
1.1. Cartilage
1.1.1. Reduced activation of chrondrocytes
1.1.1.1. Reduced production and maintainence of cartilage matrix
1.1.1.1.1. Reduced production of synovial fluid and less lubrication for articulating joints
1.1.2. Breakdown of the extracellular matrix
1.1.2.1. Breakdown of cross-linkage with collagen II (stabilized by collagen IX and XI) and glycosaminoglycans
1.2. Mechanical Stress (Krishanasamy et al., 2018)
1.2.1. Sarcopenia replaces skeletal muscle with adipose tissue (Krishnasamy, 2018)
1.2.1.1. increased adipose tissue within the muscle which is an endocrine organ that secretes inflammatory cytokines: adipokines like adiponectin, resistin, IL-1β and TNF-α (Hererro-Beaumont et al., 2018)
1.2.1.1.1. IL-1β and TNF-α activate nuclear factor kappa-light-chain to active B cell pathway which reduce activation of synovial cells and chrondrocytes (Krishnasamy, 2018)
2. inhibition of COX and reduction in production of prostaglandins that cause inflammation, swelling, fever and pain. AE: headaches, dizziness, stomach pain
3. DIAGNOSIS
3.1. 1. No lab tests for the diagnosis of OA
3.2. 2. Radiographic features: Joint space narrowing Osteophytes Subchondral cysts Subchondral sclerosis
3.3. 3. Arthrocentesis:. Shows clear fluid, No inflammatory cells.
3.4. 4. Physical examination Knees/Hips DIP joint. Bony enlargement of joints Crepitus
4. NURSING MANAGEMENT
4.1. Assessment
4.1.1. Physical Exam
4.1.1.1. ROM
4.1.1.2. Movement
4.1.1.2.1. Functional Ability
4.1.2. Skin Assessment
4.1.2.1. Color
4.1.2.2. Temperature
4.1.2.3. Integrity
4.1.2.4. Edema
4.1.2.5. Bruising, Rashes, Lesions
4.1.3. Neurological Assessment
4.1.4. Signs of deviation in body alignment and posture (Potter & Perry, 2019, p. 853)
4.1.5. Assess current client knowledge (Potter & Perry, 2019, p. 853)
4.2. Patient History
4.2.1. Injury History
4.2.2. Assessing the diet for modifications (Potter & Perry, 2019, p. 853)
4.2.2.1. Sugar Intake
4.2.2.2. Alcohol
4.2.2.3. Protein Intake
4.2.3. Exercise
4.3. Assistive Ambulatory Devices
4.3.1. Canes
4.3.2. Braces
4.3.3. Walkers
4.3.4. Shoe Inserts
4.3.5. Other Gripping/Grabbing Tools
5. LONG-TERM PROGNOSIS
5.1. Cartilage
5.1.1. Break down
5.1.2. Uneven edges
5.1.3. Cracks
5.2. Joint Replacement Surgery
5.3. Bones
5.3.1. Hardened
5.3.2. Altered Shape
5.3.3. Bumpiness
6. NURSING INTERVENTION
6.1. Lifestyle changes
6.1.1. Staying Active
6.1.1.1. Walking or Jogging
6.1.1.2. Swimming
6.1.1.3. Yoga
6.1.1.4. Bike Riding
6.1.1.5. Light Weight Training
6.1.1.5.1. Strength training has shown to increase knee extensor muscle strength by 30-40% to have an effect on reducing pain and disability (Krishnasamy, 2018)
6.1.2. Diet
6.1.2.1. OA Friendly Foods
6.1.2.1.1. Fresh Vegetables & Fruit
6.1.2.1.2. Plant Based Oils
6.1.2.1.3. Protein Rich Foods
6.1.2.1.4. Green Tea
6.1.2.1.5. Nuts
6.1.2.2. Avoid
6.1.2.2.1. Caffeine
6.1.2.2.2. Sugar
6.1.2.2.3. Salt
6.1.2.2.4. Complex Carbs
6.2. Pain Management (Kolasinski, 2020)
6.2.1. OTC Oral Analgesics
6.2.1.1. NSAIDS
6.2.1.1.1. Acetylsalicylic acid
6.2.1.1.2. Ibuprofen
6.2.1.1.3. Naproxen
6.2.1.2. Acetaminophen
6.2.2. Opioids (Not 1st choice)
6.2.2.1. Weak
6.2.2.1.1. Codeine
6.2.2.1.2. Propoxyphene
6.2.2.1.3. Tramadol
6.2.2.2. Strong
6.2.2.2.1. Oxycodone
6.2.2.2.2. Oxytrex
6.2.2.2.3. Oxymorphone
6.2.2.2.4. Fentanyl
6.2.2.2.5. Morphine Sulfate
6.2.3. Topical Ointments & Creams
6.2.3.1. Cream/Gel Analgesiscs
6.2.3.2. Capsaican Cream
6.2.3.3. Tiger Balm
6.2.3.4. Horse Liniment
6.2.3.5. Diclofenac
6.2.4. Holistic & Home Remedies
6.2.4.1. Compresses
6.2.4.1.1. Hot (Joint Stiffness)
6.2.4.1.2. Cold (Joint Pain)
6.2.4.2. Epsom Salt Baths
6.2.4.3. Supplements
6.2.4.3.1. Glucosamine
6.2.4.3.2. Chondroitin Sulfate
6.3. Rehabilitation
6.3.1. Massage
6.3.2. Physiotherapy
6.3.3. Accupuncture
6.4. Educating on family support and long-term commitment (Potter & Perry, 2019, p. 852)
7. Reduction in strength due to changes in muscle quality
8. binding to opioid receptors to prevent pain perception. AE: dizziness, constipation, poor concentration, nausea/vomiting
9. COMPLICATIONS
9.1. Sleep Disruption
9.1.1. Restlessness
9.1.2. Joint Stiffness
9.1.3. Limited ROM
9.2. Reduced Productivity
9.2.1. Weight Gain (Guss et al., 2019)
9.2.1.1. Diabetes
9.2.1.2. Hypertension
9.2.1.3. Heart Disease
9.3. Anxiety & Depression
9.4. Osteonecrosis
9.5. Pinched Nerves (OA of Spine)
9.6. Bleeding
9.6.1. Joint Infection
9.7. Stress Fractures
9.8. Rapid & Complete Cartilage Breakdown
9.8.1. Chrondolysis
10. CLINICAL MANIFESTATIONS (Rizou, Chronopoulos, Ballas & Lyritis, 2018)
10.1. Symptoms
10.1.1. Knees
10.1.1.1. Painful
10.1.1.2. "Grating" or Scraping" feeling with movement
10.1.2. Hips
10.1.2.1. Groin/buttocks pain
10.1.3. Reduced joint mobility
10.1.3.1. Muscle weakness
10.1.3.2. Joint stiffness upon waking/resting
10.1.3.3. Pain/aching with activity, after long activity or end of day
10.1.4. Feet
10.1.4.1. Big toes are painful and tender
10.1.4.2. Ankles and toe swelling
10.1.5. Neck Pain
10.2. Signs
10.2.1. Fingers
10.2.1.1. Spurs on edge of joints
10.2.1.1.1. Swollen
10.2.1.1.2. Tender
10.2.1.1.3. Redness
11. ETIOLOGY + RISK FACTORS (Palazzo, Nguyen, Lefevre-Colau, Rannou & Poiraudeau, 2016)
11.1. Hemophilia
11.1.1. Breakdown of joint cartilage and irreversible chronic arthropathy involving ankle OA (Lobet, Hermans, Bastien, Massaad & Detrembleur, 2012)
11.2. Primary OA: Age
11.2.1. Older Adults
11.2.2. Younger Adults
11.3. Genetics
11.3.1. Grandparents
11.3.1.1. Parents
11.3.1.1.1. Siblings
11.4. Primary OA: Gender
11.4.1. Female; >55 yoa (postmenopausal women)
11.5. Occupation
11.5.1. Physical Labor: Overuse of joints
11.5.1.1. Kneeling, Squatting and Climbing Stairs
11.5.1.2. Hands, Knees and Hips
11.6. Sports-related Injuries (Wong, Jayadev, Khan & Johnstone, 2012)
11.6.1. Torn Cartilage
11.6.2. Dislocated Joints
11.6.3. Ligament Injuries
11.6.3.1. Anterior Cruciate Ligament
11.7. Secondary OA: Overweight
11.7.1. Excess body weight adds stress on joints
11.7.1.1. Knees
11.7.1.2. Hips
11.7.1.3. Back
11.7.2. Fat cells promote inflammation
11.7.3. Increased body weight leads to reduced leptin levels that cause cartilage thinning and knee OA (Hererro-Beaumont et al., 2018)
