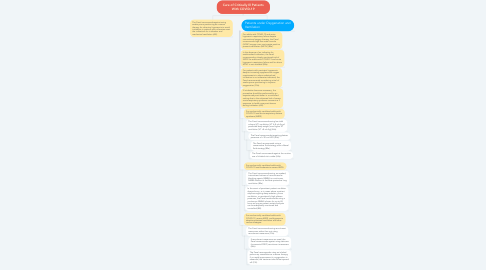
1. Patients under Oxygenation and Ventilation
1.1. For adults with COVID-19 and acute hypoxemic respiratory failure despite conventional oxygen therapy, the Panel recommends high-flow nasal cannula (HFNC) oxygen over noninvasive positive pressure ventilation (NIPPV) (BIIa).
1.2. In the absence of an indication for endotracheal intubation, the Panel recommends a closely monitored trial of NIPPV for adults with COVID-19 and acute hypoxemic respiratory failure and for whom HFNC is not available (BIIa).
1.3. For patients with persistent hypoxemia despite increasing supplemental oxygen requirements in whom endotracheal intubation is not otherwise indicated, the Panel recommends considering a trial of awake prone positioning to improve oxygenation (CIIa).
1.4. If intubation becomes necessary, the procedure should be performed by an experienced practitioner in a controlled setting due to the enhanced risk of severe acute respiratory syndrome coronavirus 2 exposure to health care practitioners during intubation (AIII).
1.5. For mechanically ventilated adults with COVID-19 and acute respiratory distress syndrome (ARDS)
1.5.1. The Panel recommends using low tidal volume (VT) ventilation (VT 4–8 mL/kg of predicted body weight) over higher VT ventilation (VT >8 mL/kg) (AIIa).
1.5.1.1. The Panel recommends targeting plateau pressures of <30 cm H2O (AIIa).
1.5.1.1.1. The Panel recommends using a conservative fluid strategy over a liberal fluid strategy (BIIa).
1.6. For mechanically ventilated adults with COVID-19 and moderate-to-severe ARDS:
1.6.1. The Panel recommends using, as needed, intermittent boluses of neuromuscular blocking agents (NMBA) or continuous NMBA infusion to facilitate protective lung ventilation (BIIa).
1.6.1.1. In the event of persistent patient-ventilator dyssynchrony, or in cases where a patient requires ongoing deep sedation, prone ventilation, or persistently high plateau pressures, the Panel recommends using a continuous NMBA infusion for up to 48 hours as long as patient anxiety and pain can be adequately monitored and controlled (BIII).
1.7. For mechanically ventilated adults with COVID-19, severe ARDS, and hypoxemia despite optimized ventilation and other rescue strategies:
1.7.1. The Panel recommends using recruitment maneuvers rather than not using recruitment maneuvers (CIIa).
1.7.1.1. If recruitment maneuvers are used, the Panel recommends against using staircase (incremental PEEP) recruitment maneuvers (AIIa).
1.7.1.1.1. The Panel recommends using an inhaled pulmonary vasodilator as a rescue therapy; if no rapid improvement in oxygenation is observed, the treatment should be tapered off (CIII).
