1. nutrition assessment
1.1. water
1.1.1. body needs minimum 1500 mL to replace what its used.
1.1.2. thirst is a late sign of dehydration
1.2. favorites?
1.3. typical days food
1.4. how much of each they mention
1.5. social things like access to transportation, income,
1.6. physical assessment
1.6.1. cachexia-skin thin?
1.6.2. nails
1.6.3. fatigue
1.6.4. enlarged spleen
1.6.5. skin
1.7. labs- nitrogen, albumen, urine output, color, odor
1.8. religious factors
1.9. healthy bmi: 18.5-24.5, overweight 24.5-29.5, obese: over 30
1.10. food preparation: does the patient understand safe food prep, age appropriate foods.
1.10.1. raw chicken, cut grapes for kids
1.10.2. at risk pops for food borne illness: immunocompromised, kids, elderly
2. pregnancy
2.1. Folate intake during pregnancy
2.1.1. prevent neural tube defects
2.1.2. 400 mcg a day
2.1.3. deficient can lead to neural tube defect
2.1.4. pregnant women should consume folate-rich foods such as asparagus, spinach and broccoli. Supplemental folic acid may be needed.
2.2. Fiber intake during pregnancy
2.2.1. f
2.2.2. 25- 30 grams per day
2.2.3. prevents constipation during pregnancy
2.2.3.1. can lead to hemorrhoids
2.2.4. sources
2.2.5. second tri bump up calories 340 or 350 calories per day
2.2.6. third tri bump up about 450 calories per day
2.3. Calculating appropriate intake of fat calories per day
2.3.1. About 20% to 35% total calories from fat per day
2.3.2. 9 calories per gram
2.3.3. good and bad fats, LDL, HDL
2.3.4. make up cell walls
2.3.5. hdl removes excess cholesterol, LDL takes cholesterol to the cells
3. Types of Protein
3.1. storage proteins
3.2. Amino acids
3.3. complete and incomplete
3.4. complete have all aminos, incomplete do not
3.5. help with wound healing
4. Teaching about vitamins & minerals
4.1. Can get vitamins and minerals from supplements
4.1.1. fat soluble A,D,E,K
4.1.1.1. D- from the sun
4.1.1.2. vitamin K for clotting, we give to babys when born
4.1.1.3. D and C important for immunity
4.2. Can get vitamins and minerals from food
4.3. vitamins are fat soluble or water soluble
4.3.1. water soluble B and C
4.4. Vitamin C helps in immunity
4.5. deficient electrolytes can affect major organs
4.5.1. potassium- heart
4.5.2. calcium- muscle contraction
5. infants
5.1. breast milk alone for 6 months minimum
5.2. storage of milk
5.3. never boil or microwave
5.4. avoid water tox with distilled water
5.5. low income? are they rationing their formula
5.6. one at a time foods when introducing
6. Indications of dietary deficiency
6.1. fatigue
6.2. dizziness
6.2.1. decreased vision
6.3. wt loss
6.4. slow growth
6.5. loss of muscle
6.5.1. muscle twitching
6.6. weakness
6.7. swollen red tongue
6.8. bone loss
6.9. in kids: rickets,
6.10. slow healing
6.11. Skin tenting
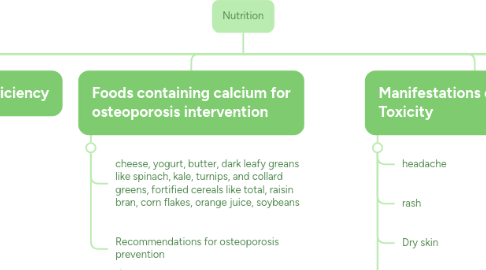
7. Foods containing calcium for osteoporosis intervention
7.1. cheese, yogurt, butter, dark leafy greans like spinach, kale, turnips, and collard greens, fortified cereals like total, raisin bran, corn flakes, orange juice, soybeans
7.2. Recommendations for osteoporosis prevention
7.2.1. depoprovera birthcontrol is a risk factor for osteoporosis
7.2.2. adequate exercise and weight bearing activities help keep bones healthy
7.2.3. medications are a risk factor
8. Manifestations of Vitamin A Toxicity
8.1. headache
8.2. rash
8.3. Dry skin
8.4. Impaired vision
8.5. Dry eyes
9. Teaching about sources of protein
9.1. Teaching about sources of protein
9.2. meat, fish, beans,
9.3. Egg/egg whiite
9.4. all 9 aminos
9.5. complete and incomplete. if no meat in diet a person needs to intake beans and rice to get all aminos
10. Teaching about sources of fiber
10.1. Teaching about sources of fiber
10.1.1. beans
10.1.1.1. brown rice
10.1.2. whole grains
10.1.3. bran cereal
10.1.4. Green leafy vegetables
10.1.5. 28 g for women 38 for men
10.1.6. indigestible, helps with defacation
11. therapeutic diets
11.1. full liquid
11.2. pureed
11.3. soft-bland low fiber
11.4. mechanical soft
11.5. dysphagia
11.6. clear liquid
11.7. types of people
11.7.1. stroke
11.7.2. extubation
11.7.3. GI patients
11.7.3.1. avoid caffeine
11.7.3.2. gerd
11.7.3.3. colitis
11.7.3.4. n/v/d
11.7.3.5. electrolyte imbalances
11.7.3.5.1. IV replaces volume
11.7.3.5.2. pedialyte
11.7.3.6. diverticulitis/osis
11.7.3.7. celiac
11.7.3.7.1. avoid gluten
11.7.3.7.2. can have rice
11.7.4. post op
11.7.5. renal patients
11.7.5.1. avoid high protein/phosphorus
11.7.5.2. intake and output
11.8. immunocompromised
11.8.1. consider they are at risk for infection
11.8.2. watch you shelf life on foods
11.8.3. food prep and storage and its source
