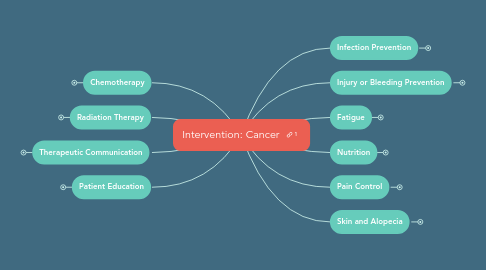
1. Chemotherapy
1.1. Chemo administration
1.1.1. PPE
1.1.1.1. Mixing or administering IV or PO chemo
1.1.1.2. Handling patients' excreta receiving chemo x 48 hours
1.2. Chemo-induced N/V
1.2.1. Administer antiemetic BEFORE chemo
1.3. Prevent extravasation
1.3.1. Stop infusion if...
1.3.1.1. Patient complains of pain (e.g., burning, stinging) during chemo
1.3.1.2. Site is red, tender, and swelling
1.3.2. Prevention
1.3.2.1. Infuse chemo via central line
1.3.2.2. Use bigger gauge IV (e.g., 16 or 18)
1.3.2.3. Flush the line before and after medication administration
1.3.3. Treatment
1.3.3.1. Elevate the extremity
1.3.3.2. Apply cold compress
1.3.3.3. Attempt to aspirate the vesicant
1.3.3.4. Contact the provider for pharmacological treatment
1.4. Question
1.4.1. The nurse is administering a vesicant chemotherapy agent to a patient who has colon cancer. During rounds, the nurse notes that the intravenous site is reddened and swollen, and the patient reports that it is painful. What is the first action the nurse will take?
1.4.1.1. a. Turn off the infusion.
1.4.1.2. b. Slow the infusion rate.
1.4.1.3. c. Check the patient's vital signs.
1.4.1.4. d. Notify the primary health care provider.
2. Radiation Therapy
2.1. Teletherapy
2.1.1. Avoid removing the radiation markings
2.1.2. Avoid sun exposure to the radiation site
2.1.3. Patient is NOT radioactive after the procedure
2.2. Brachytherapy
2.2.1. Temporary vs. permanent implants
2.2.1.1. Temporary
2.2.1.1.1. May last one to few days
2.2.1.1.2. Patient may need to stay in bed
2.2.1.2. Permanent
2.2.1.2.1. Last weeks to months
2.2.2. Minimize radiation exposure
2.2.2.1. Private room and private bath
2.2.2.2. Keep door closed as much as possible
2.2.2.3. Portable lead shields
2.2.2.4. Wear a lead apron when providing care
2.2.2.5. Wear a dosimeter film badge
2.2.2.5.1. Measure a person's exposure to radiation
2.2.2.5.2. Never share dosimeter film badge
2.2.2.6. Nurses who are pregnant should not care for the patient
2.2.3. Handling radioactive source
2.2.3.1. Never use bare hands
2.2.3.2. Use long-handled forceps
2.2.3.3. Deposit the source in the lead container
2.2.4. Visitors
2.2.4.1. Limit the number of visiting hour
2.2.4.2. 6 feet away from the patient
2.2.4.3. Pregnant women and children are not allowed
2.3. Questions
2.3.1. Question 1
2.3.1.1. The patient is being treated with brachytherapy for cervical cancer. What factors of protection must the nurse be aware of when caring for this patient?
2.3.1.1.1. a. The medications the patient is taking
2.3.1.1.2. b. The nutritional supplements that will help the patient
2.3.1.1.3. c. How much time is needed to provide the patient's care
2.3.1.1.4. d. The time the nurse spends with the patient and at what distance
2.3.2. Question 2
2.3.2.1. The nurse provides instructions regarding markings on the skin to a patient who is undergoing radiation therapy. What explanation should the nurse provide regarding the markings?
2.3.2.1.1. a. They are permanent effects of radiation therapy.
2.3.2.1.2. b. They indicate that previous treatments have been unsuccessful.
2.3.2.1.3. c. They are a warning of potentially serious side effects of radiation.
2.3.2.1.4. d. They should be protected because they are landmarks for the radiation therapy.
2.3.3. Question 3
2.3.3.1. A nurse is caring for a patient undergoing brachytherapy for prostate cancer. What actions should the nurse take to protect themselves from radiation hazards? Select all that apply.
2.3.3.1.1. a. Use shielding when providing any care to the patient.
2.3.3.1.2. b. Organize care to limit the time spent in direct contact with the patient.
2.3.3.1.3. c. Share the film badge with a colleague who forgot his or her own badge.
2.3.3.1.4. d. Wear the film badge at all places of work to indicate your nature of work.
2.3.3.1.5. e. Limit close proximity to the patient to only those care tasks that must be performed near the source.
3. Therapeutic Communication
3.1. Diagnosis of CA may not be a "death sentence"
3.2. Provide support
3.2.1. Active listening
3.2.2. Demonstrate emphathy
3.2.3. Use silence
4. Patient Education
4.1. Cancer prevention
4.1.1. Primary prevention
4.1.1.1. Avoid exposure to carcinogens
4.1.1.2. Modifying associated risk factors
4.1.1.3. Vaccination
4.1.1.4. Seven warning signs of CA
4.1.2. Secondary prevention
4.1.2.1. Screening
4.1.2.1.1. Breast CA
4.1.2.1.2. Colorectal CA
4.1.2.1.3. Cervical CA
4.1.2.1.4. Prostate CA
5. Infection Prevention
5.1. Neutropenic precaution
5.1.1. Private room
5.1.2. Hand hygiene
5.1.3. Strict aseptic technique
5.1.4. Appropriate PPE
5.1.5. Limit the number of healthcare personnel & visitors
5.1.6. Avoid uncooked food, fresh flowers, plants
5.1.7. Notify the provider for S/S of infection
6. Injury or Bleeding Prevention
6.1. Handle the patient gently
6.2. Use lift sheet when moving or positioning
6.3. Avoid IM injections or venipunctures
6.4. Apply firm pressure to needle sticks site for 10 minutes
6.5. Apply ice to areas of trauma
6.6. Avoid trauma to rectal tissues (e.g., enemas, suppositories)
6.7. Teach the use of electric shaver than a razor
6.8. Use a soft-bristled toothbrush or tooth sponges
6.9. Avoid blowing the nose or insert objects into the nose
6.10. Fall prevention (e.g., non-skid socks, side rails up, walkways clear and uncluttered)
7. Fatigue
7.1. Pace activities with rest and conserve energy
7.2. Improve sleep quality and quantity
7.3. Question
7.3.1. When caring for a patient undergoing chemotherapy, which nursing actions should the nurse take to manage fatigue in the patient? Select all that apply.
7.3.1.1. a. Pace activities in accordance with energy level.
7.3.1.2. b. Encourage strenuous exercise to build strength.
7.3.1.3. c. Encourage the patient to be active even when tired.
7.3.1.4. d. Maintain usual lifestyle patterns as much as possible.
7.3.1.5. e. Reassure the patient that fatigue is a common side effect.
8. Nutrition
8.1. Xerostomia
8.1.1. Use salivary stimulant (chewing gum, biotene)
8.1.2. Increase fluid intake
8.1.3. Moisten the food with liquids or gravies
8.1.4. Sipping liquids between meals
8.1.5. Lubricate lips
8.2. Dysphagia
8.2.1. Position the patient in high-Fowler during feeding and eating
8.2.2. Provide time to eat, chew, and swallow
8.2.3. Provide small bites
8.2.4. Thicken the liquids as prescribed
8.2.5. Have suction ready in the room
8.3. Mucositis
8.3.1. Oral hygiene and dental care
8.3.2. Ice chips, popsicles
8.3.3. Soft, bland, high-calorie, high-protein diet
8.3.3.1. Avoid spicy, salty, acidic, dry, rough, hard food
8.4. Taste alterations
8.4.1. Use aromatic food and spices
8.4.2. Oral hygiene before food
8.5. Anorexia
8.5.1. Encourage food choices
8.5.2. High-calorie and high-protein food
8.5.3. Supplemental nutrition, enteral or parenteral nutrition
8.6. N/V
8.6.1. Avoid triggers
8.6.2. Antiemetic before meals
8.7. Questions
8.7.1. Question 1
8.7.1.1. A nurse is caring for a patient with lung cancer who is being treated with chemotherapy. The patient reports anorexia. How should the nurse ensure an adequate nutritional status of the patient? Select all that apply.
8.7.1.1.1. a. Provide large meals.
8.7.1.1.2. b. Weigh the patient weekly.
8.7.1.1.3. c. Provide nutritional supplements.
8.7.1.1.4. d. Provide high-calorie, high-protein food.
8.7.1.1.5. Manage nausea and vomiting if present.
8.7.2. Question 2
8.7.2.1. A nurse is caring for a patient experiencing severe side effects of chemotherapy. On examination, the nurse notices stomatitis. Which interventions should the nurse perform to relieve stomatitis? Select all that apply.
8.7.2.1.1. a. Apply topical anesthetics.
8.7.2.1.2. b. Encourage nutritional supplements.
8.7.2.1.3. c. Give diuretics and laxatives regularly.
8.7.2.1.4. d. Encourage oral application of alcohol.
8.7.2.1.5. e. Discourage the use of oral irritants like tobacco.
9. Pain Control
9.1. Pharmacological
9.2. Non-pharmacological
10. Skin and Alopecia
10.1. Skin desquamation
10.1.1. Protect from UV light
10.1.2. Avoid applying heat and cold pads
10.2. Strategies to improve appearance
10.3. Avoid scalp injury
10.4. Question
10.4.1. A nurse assesses that a patient undergoing radiotherapy has developed erythema and desquamation. Which should the nurse include when educating the patient about skin care in the radiation treatment area?
10.4.1.1. a. Use perfumes and cosmetics on the treatment area as desired.
10.4.1.2. b. Wear fabrics such as wool and corduroy to prevent exposure to cold.
10.4.1.3. c. Gently cleanse the skin using a mild soap, tepid water, and a soft cloth.
10.4.1.4. d. Allow brief periods of direct exposure to sunlight for good bone health.
