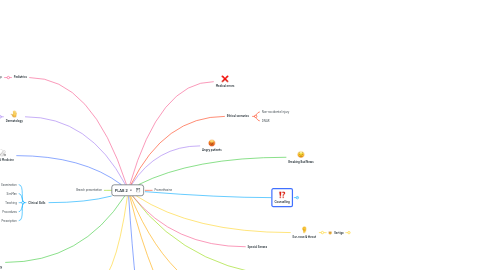
1. Pediatrics
1.1. Cradle Cap
2. Dermatology
2.1. Skin Growth
2.1.1. Basal cell carcinoma
2.1.1.1. No need for radiotherapy or chemotherapy
2.1.2. Squamous cell carcinoma
2.1.2.1. Comes with immunosupression
2.1.3. Melanoma
2.1.4. Benign mole
2.1.4.1. Epidermoid cyst
2.1.4.2. Lipoma
2.1.4.3. Sebhorric keratosis
2.1.4.4. Benign mole
2.2. Important ones
2.2.1. Paoriasis
2.3. Rashes
2.3.1. Cholinergic urticaria
2.3.2. Eczema (atopic dermatitis)
2.3.3. Impetigo
2.3.3.1. Infect for 48 hours after appearance
2.3.4. Herpes labialis (cold sores)
2.3.5. Acne vulgaris
2.3.5.1. Avoid picking or scratching for marks
2.3.5.2. Treated by lotion of topical retinoid and benzyol peroxide
2.3.6. Tinea mannum (of the body)
2.3.6.1. Clotrimazol for 4 weeks 2-3 times a day
2.3.7. Tinea capitis (of the head)
2.3.7.1. DANDRUFF
2.3.7.2. Treatment
2.3.7.2.1. Griseofulvin
2.3.7.2.2. Ketoconazole shampoo for 4 to 8 week, use 2 to 3 times weekly
2.3.8. Tines pedis (of the feet)
2.3.8.1. Runners feet due to sweating
2.3.8.1.1. Clotrimazole cream for 1-2 weeks
2.3.8.1.2. Hydrocortisone cream
2.3.9. Scabies
2.3.9.1. Overcrowding and bad hygiene
2.3.9.2. Associated with burrows
2.3.10. Measles
2.3.10.1. Infective for 4 days after the onset of rash
2.3.10.2. Ask about vaccination and give vaccination MMR after it reaolves
2.3.10.3. Koplik spots inside the mouth
2.3.10.4. NOTIFIABLE DISEASE 📣
2.3.10.5. FFR
2.3.11. Hemangioma
2.3.12. Cellulitis
2.3.12.1. Doxycycline
2.3.13. Paronychia
2.3.13.1. Fucidic acid
2.3.13.2. Avoid tight shoes
2.3.14. Chickenpox (Varicella Zoster Virus)
2.3.14.1. Treatment
2.3.14.1.1. FFR
2.3.14.1.2. Lactocalamine solution
2.3.14.2. Infectivity period: 2 days before the rash & 5 days after
2.3.15. Intretigo
2.3.15.1. Clotrimazole & hydrocortisone cream
2.3.15.2. Ringworm infection
2.3.16. Lichen sclerosus
2.3.16.1. Precursor for vuvlar cancer
2.3.16.1.1. Extensive surgery: removal of vulva, vagina, womb
2.3.16.1.2. Chemoradiotherapy
2.3.17. Genital warts
2.3.17.1. 15 years old girl
2.3.17.1.1. Caused by HPV virus
2.3.17.1.2. Relation with counselor at school
2.3.18. Cherry Angioma🍒
2.3.18.1. They normally come with age and they are vascular in origin
2.3.19. Herpetic whitlow
2.3.19.1. Mostly immunosuppressed
2.3.19.2. Can give acyclovir if less than 48 hours since it developed
2.3.19.3. Blistering
3. Internal Medicine
3.1. Cardiology
3.1.1. Stable Angina
3.1.1.1. Medical Treatment
3.1.1.1.1. GTN sublingual tablet before attacks
3.1.1.1.2. Aspirin 75mg OD / Clopidogrel
3.1.1.2. Non Medical Treatment
3.1.1.2.1. Diet, exercise, smoking cessation, & alcohol reduction to <14 units per week
3.1.1.2.2. Sexual activity
3.1.1.2.3. Inform DVLA
3.2. Endocrinology
3.3. Respiratory
3.4. Gastroenterology
3.5. Neurology
3.5.1. Headaches
3.5.1.1. Tension headache
3.5.1.2. Migraine
3.5.1.3. Subarachnoid hemorrhage
3.5.1.4. Medication overuse headache
3.5.1.5. Hangover headache
3.5.2. Meningitis 🧠🌡️
3.5.3. Seizures 🧠⚡️
4. Clinical Skills
4.1. Examination
4.2. SimMan
4.3. Teaching
4.4. Procedures
4.5. Prescription
5. Psychiatry
5.1. IMPORTANT
5.1.1. **Starting the diagnosis like**
5.1.1.1. What you might be experiencing is a mental health condition that's called
5.2. **Mini Mental State Examination (MMSE-22)**
5.3. Generalized Anxiety Disorder (GAD)
5.3.1. Presesntation
5.3.1.1. Boss at work commenting about careless mistakes **&** having difficulty concentrating
5.3.2. Ask about symptoms
5.3.2.1. Do you feel that something bad is about to happen? (Impending doom)
5.3.2.2. Do you feel annoyed/restless?
5.3.2.3. Have trouble relaxing?
5.3.2.4. Worry too much about different things?
5.3.2.5. Do you feel you cannot stop your worries?
5.3.2.6. Feeling on the edge?
5.3.3. GAD Differential Diagnosis
5.3.3.1. **PTSD**
5.3.3.1.1. Ask about certain stressful event that preceeded this feeling
5.3.3.2. **Depression**
5.3.3.2.1. Ask about the mood
5.3.3.3. **OCD**
5.3.3.3.1. Do you have any specific thoughts about objects around you?
5.3.3.3.2. Do you have any special thoughts that annoy you?
5.3.3.3.3. Do you wash or check cleanliness excessively?
5.3.3.4. **Phobias**
5.3.3.4.1. Do you fear social gatherings? or stray away from them? (social anxiety disorder)
5.3.3.4.2. Do you have any fears of certain objects or patterns?
5.3.3.4.3. **or more frankly:** do you have any specific phobias?
5.3.3.5. ADHD
5.3.3.5.1. Do you have any trouble concentrating at work/school only?
5.3.3.6. **Panic Attack **
5.3.3.6.1. Did you have any panic attacks?
5.3.4. Management
5.3.4.1. Defined as
5.3.4.1.1. Fealing excessive, unrealistic, out-of-proportion worry towards many risks.
5.3.4.1.2. Lacking control over such worries
5.3.4.2. **Alpha, beta, gamma scheme for psychiatry**
5.4. **Attention-Deficit Hyperactivity Disorder (ADHD)**
5.4.1. Lack of insight that the patient comes referred from his school
5.4.2. **10 Criteria Questions**
5.4.2.1. **5 about inattention**
5.4.2.2. 5 about hyperactivity
5.5. **Post-Traumatic Stress Disorder (PTSD)**
5.5.1. Presentation
5.5.1.1. Patient presents after having experienced a taxi crash, where the taxi driver died and her friend is currently in a coma
5.5.1.1.1. Express sympathy for friend
5.5.1.1.2. Empathize with the patient as this is a stressful event & you are here to help them
5.5.1.2. **And sleeping difficulty**
5.5.2. Trauma-Screening Questionnaire (TSQ) (10 QUESTIONS)
5.5.2.1. 5 Memory Questions
5.5.2.1.1. Daytime flashbacks of upsetting events
5.5.2.1.2. Nightime nightmares
5.5.2.1.3. Angry reminder: Get upset/angry when reminded of the event
5.5.2.1.4. Physical: Get physical symptoms when they get reminded
5.5.2.1.5. Aniticipate: Feel the same event is going to happen again
5.5.2.2. 5 Arousal Questions
5.5.2.2.1. Sleeping difficulty: falling or maintaining
5.5.2.2.2. Concentration difficulty
5.5.2.2.3. Irritable or easily angered
5.5.2.2.4. High alertness towards potential dangers
5.5.2.2.5. Jumpy or startled by unexpected events (loud sudden noises might annoy)
5.5.2.3. **Scoring 6 yes, yes being happening at least twice in the last week >> PTSD diagnosis**
5.5.3. Ask about
5.5.3.1. Detachment from surrounding people
5.5.3.2. Feeling numb
5.5.3.3. Feeling worthless
5.5.3.4. Feeling negative
5.5.3.5. Assess suicidal risk
5.5.3.6. Effect on life, work, relationships, communication with others, thoughts
5.5.4. Differential diagnosis
5.5.5. Management
5.5.5.1. Definition
5.5.5.1.1. When someone being part or witnesses a stressful event or an accident, this person might get upsetting flashbacks and nightmares of the event, and thoughts that can be uncontrollable that can interfere with everyday activities
5.5.5.2. **URGENT** referral to specialist
5.5.5.2.1. Psychotherapy
5.5.5.2.2. Pharmacotherapy
5.5.5.3. Give short-term hypnotics **(SLEEPING PILLS)**
5.5.5.3.1. only PLAB 2 situation for the use of short-term hypnotics, beside domestic violence woman coming with sleeping problems
5.5.5.3.2. Safety net about
5.6. Obessessive Compulsive Disorder (OCD)
5.6.1. **Presentation**
5.6.1.1. Medical intern/student that comes to you worried about contracting an infection in the hospital
5.6.1.1.1. **FIRST:** check why does the intern/student thinks like that
5.6.1.2. Time consuming and affecting the patient
5.6.2. **Questions to be asked**
5.6.2.1. Do you **wash** or clean a lot?
5.6.2.2. Do you **check** things a lot?
5.6.2.3. Is there any **thought** that keeps bothering you that you would like to get rid of, but cannot?
5.6.2.4. Do your **daily activities** take a long time to finish?
5.6.2.5. Are you concerned about **putting things in a special order,** or are you upset by mess?
5.6.2.6. Do these problems **trouble ** you? (insight)
5.6.2.7. **Assess effect**
5.6.2.7.1. How are those thoughts and actions affecting your life?
5.6.2.7.2. How many times per day?
5.6.2.7.3. How much of the day is consumed in such actions?
5.6.3. **Remember to do examination (hand and eyes)**
5.6.3.1. Patient might be washing excessively that can cause eczema
5.6.4. Management
5.6.4.1. Definition
5.6.4.1.1. **all about stating what are obsessions and how they cause compulsions**
5.6.4.1.2. People with this condition experience a pattern of unwanted thoughts and fears that are called **obsessions**. Those obsessions lead to doing repetitive actions that are called **compulsions** causing affection to daily activities and causing distress
5.6.4.2. Referral to specialist
5.6.4.2.1. CBT
5.6.4.2.2. Pharmacotherapy
5.6.4.2.3. If severe: DEEP BRAIN STIMULATION (that's a surgery)
5.7. **New Depression 2 Cases**
5.7.1. Post angina & stenting depression
5.7.1.1. nurse visited to find patient no taking medications
5.7.1.2. Patient tells: I do not want to take medications
5.7.1.3. Management
5.7.1.3.1. Moderate depression
5.7.2. Not getting better on SSRI
5.7.2.1. Give SSRI
5.7.2.1.1. Side effects: sexual dysfunction, excessive sweating, tummy pain, constipation
5.7.2.2. Give **RUBOXETINE** if patient is worried about sexual dysfunction
6. Herpes
6.1. Herpes labialis
6.2. Genital herpes
6.3. Herpetic whitlow
7. Angry patients
8. Medical errors
9. Ethical scenarios
9.1. Non-accidental injury
9.2. DNAR
10. Ophthalmology
10.1. Age Related Macular Degeneration (ARMD)
10.1.1. Wavy lines and blurry vision for 3-4 months
10.1.2. Types
10.1.2.1. Dry ARMD
10.1.2.2. Wet ARMD
10.1.2.2.1. Treatable with eye injections
10.1.3. Was at the optometrist
10.1.4. Referral within a day to ophthalmologist
10.1.4.1. Slit lamp, fluorescein angiography, Ocular coherence tomography
10.1.5. Lifestyle modifications, diet and exercise
10.2. Cataract
10.2.1. Opacification of the lens leading to gradual blurriness and cloudiness
10.2.2. Cloudy vision, glare around light >> both occur gradually
10.2.3. Management
10.2.3.1. Opthalmologist referral routine?
10.2.3.1.1. For surgery, capsule removal
10.2.3.2. Optometrist for visual acuity assessment
10.2.3.3. Advice for driving: daylight and good visual acuity >> DVLA inform
10.3. Angel Closure Glaucoma
10.3.1. Painful eye, sudden onset
10.3.2. Never ever ever do fundoscopy
10.3.3. Eye pressure test (Tonometry)
10.3.4. **Management**
10.3.4.1. Admission
10.3.4.2. Opthalmologist assessment
10.3.4.2.1. **Pressure-lowering medications: ** Pilocarpine eye drops + Acetazolamide
10.3.4.2.2. Gonisocopy + Slit Lamp
10.3.4.2.3. Peripheral iridotomy using laser device to ↓ pressure
10.3.4.3. **CAUSE: Patient taking amitriptyline**
10.4. Open-Angle Glaucoma
10.4.1. Patchy blind spots
10.4.2. **Management**
10.4.2.1. Ophthalmologist referral
10.4.2.1.1. Gonioscopy, visual field test, optic nerve assessment
10.4.2.1.2. Selective laser trabeculoplasty
10.4.2.1.3. Trabeculotomy
10.5. Toxoplasmosis
10.5.1. Pigmented retinal scarring present on fundoscopy
10.5.2. Most people get better without ttt
10.5.3. but need ttt if pregnant or immunocompromised
10.5.3.1. Pyrimethamine
10.5.3.2. Sulfadiazine
10.5.4. Infectious disease referral
10.6. Scleritis
10.6.1. Associated with old lady that has rheumatoid arthritis
10.6.2. Presentation
10.6.2.1. Dull eye pain
10.6.2.2. **Photophobia**
10.6.2.2.1. Beware that this is photophia with eye pain and no fever
10.6.2.2.2. Meningitis is photophobia (fearing light/shying away from light) with neck pain and fever ± contact with infected person
10.6.3. Urgent ophthalmology referral **(within 24 hours)**
10.6.3.1. Slit lamp test
10.6.3.2. NSAIDs then oral steroids
10.6.4. Routine rheumatology referral
10.7. Giant Cell Arteritis
10.7.1. Temporal artery arteritis, might be affecting eye sight
10.7.2. Medical Emergency
10.7.3. With visual loss
10.7.3.1. urgent (same day) referral to ophthalmology
10.7.3.1.1. IV Glucocorticoids, if not oral 60-100mg
10.7.4. Without visual affection
10.7.4.1. urgent assessment by rheumatologist
10.7.5. Treatment for 1-2 years
10.8. Ocular herpes
10.8.1. Urgent same day referral to ophthalmologist
10.8.2. Herpes virus lies dormant in the nerves and can travel down them causing reinfection
10.8.3. Safety net on recurrent infections'
10.8.3.1. If recurrent infection take antiviral tablets every day
10.8.3.2. Can cause complications
10.8.4. Avoid wearing contactlenses
10.9. Blepharitis
10.9.1. Inflammation of the eyelids by infection or allergin
10.9.1.1. flaky crustings on the tip of the eyelid
10.9.1.2. Gritty and itchy and painful
10.9.2. Artificial teardrops & Doxycycline drops or eye ointment
10.9.3. Keep good eyelid hygiene
10.9.4. Avoid wearing contact lenses and eye make up like eyeliners and mascara
10.10. Stye
10.10.1. Inflammation of the apocrine or sebaceious glands due to bacterial infection
10.10.1.1. Internal stye can develop to meibomian cyst
10.10.1.2. External stye
10.10.2. Self limiting condition in 1-2 weeks
10.10.3. Keep good eyelid hygiene
10.10.4. Avoid wearing contact lenses and eye make up like eyeliners and mascara
10.11. Keratitis
10.11.1. Inflamed cornea
10.11.2. Can be caused by lenses that are unhygienic
10.11.3. Immediate referral to ophthalmologis as medical emergency
10.11.3.1. Slit lamp exam
10.11.3.2. Corneal scrapping
10.11.3.3. Intensive systemic ABX
10.11.3.4. Topical doxycycline or gentamycin
11. Ear, nose & throat
11.1. Vertigo
11.1.1. Meniere's Disease
11.1.1.1. Vertigo episodes that last from 20 minutes to 12-24 hours
11.1.1.1.1. Unilateral
11.1.1.1.2. Aural fullness
11.1.1.1.3. Roaring tinnitus
11.1.1.2. Immediate referral to ear clinic
11.1.1.3. Multidisciplinary team management
11.1.2. Benign Paroxysmal Positional vertigo (BPPV)
11.1.2.1. Episodic vertigo lasting for seconds (30s)
11.1.2.1.1. results from dislodgement of calcium carbonate otoconia in the semicircular canals (posterior most commonly)
11.1.2.1.2. related to sudden head movements **(positional)**
11.1.2.2. **Positive Dix-Hallpike test**
11.1.2.3. Management
11.1.2.3.1. Self-limiting & reassurance
11.1.2.3.2. Symptomatic
11.1.2.3.3. Epley's Manoeuvre & Semont's Manoeuver
11.1.3. Vestibular Neuritis
11.1.3.1. Acute, prolonged, isolated, spontaneous vertigo
11.1.3.2. Management
11.1.3.2.1. Symptomatic
11.1.3.2.2. Self-limiting & reassurance
11.1.3.2.3. bed rest
11.1.4. Acoustic Neuroma
11.1.4.1. Urgent referral to specialist 2WW pathway
11.1.4.2. If there's a neurologic affection
11.1.4.2.1. Immediate referral
12. Emergency Medicine
13. Breaking Bad News
14. **Important Concepts**
14.1. Duty of Candor
15. Obstetrics & Gynaecology
15.1. Histories
15.1.1. Pre-eclampsia
15.1.1.1. 36 Weeks Case
15.1.2. Booking visit
15.1.2.1. Basic testing
15.1.3. Contraception
15.1.3.1. Normal contraception counseling
15.1.3.1.1. Counsel about different means of contraception
15.1.3.2. 15 years old contraception (+abuse)
15.1.3.3. Monring after pill (Learning Disability)
15.1.4. Endometritis
15.1.5. Endometriosis
15.1.5.1. First presentation endometriosis
15.1.5.2. Follow up endometriosis
15.1.5.2.1. OCP prescribed before
15.1.6. Pelvic Inflammatory Disease
15.1.6.1. Presenting by RIF pain
15.1.7. Preconception Counseling
15.1.7.1. Lesbian Counseling
15.2. Antenatal Examination
16. Counselling
16.1. Vaccinations
16.2. Pap smear
16.3. PSA
16.3.1. Friend has had been diagnosed with prostate cancer Golf ⛳️
16.3.2. Family history of prostate cancer
16.4. Vascular dementia
16.5. Stroke risk
16.5.1. Q risk assessment
16.6. Requesting postmortem
16.7. Confidentialty
16.7.1. Mother-daughter deprssion asking about diagnosis
16.7.2. Mother-daughter contraceptive pills 15 years old
16.7.3. Consultant son asking about mother’s diagnosis
16.8. Frequent bouts of illness
16.9. Surgical abortion
16.10. Lesbian wanting pregnancy 🤰🏳️🌈
16.11. Obesity 🚛
16.12. DNACPR 😵
17. **New Cases**
17.1. Cradle Cap
17.2. Counselling about pregnancy for a lesbian lady
17.3. Obesity counseling
18. Notifiable conditions
18.1. Syphilis
18.2. Measles
18.3. Benign mole
18.4. Benign mole
19. **Special Senses**
20. Promethazine
21. Problem with colleague
21.1. Delayed discharge letter
21.1.1. coaching scenario
