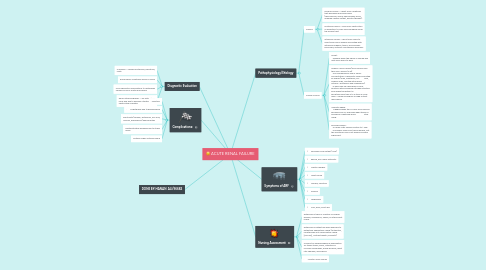
1. Diagnostic Evaluation
1.1. Urinalysis —reveals proteinuria, hematuria, casts
1.2. Rising serum creatinine and BUN levels
1.3. Urine chemistry examinations to distinguish various forms of acute renal failure
1.4. Renal ultrasonography —for estimate of renal size and to exclude a treatable obstructive uropathy
2. Complications:
2.1. . Infection
2.2. . Arrhythmias due to hyperkalemia
2.3. Electrolyte (sodium, potassium, uric acid, calcium, phosphorus) abnormalities
2.4. Gastrointestinal bleeding due to stress ulcers
2.5. Multiple organ systems failure
3. DONE BY:HANAN ALI/96682
4. Pathophysiology/Etiology
4.1. Causes
4.1.1. Prerenal causes —result from conditions that decrease renal blood flow (hypovolemia, shock, hemorrhage, burns, impaired cardiac output, diuretic therapy).
4.1.2. Postrenal causes —arise from obstruction or disruption to urine flow anywhere along the urinary tract
4.1.3. Intrarenal causes —result from injury to renal tissue and is usually associated with intrarenal ischemia, toxins, immunologic processes, systemic and vascular disorders.
4.2. Clinical Course
4.2.1. Onset : a.Begins when the kidney is injured and lasts from hours to days.
4.2.2. Oliguric–anuric phase (urine volume less than 400–500mL/24h) a.Accompanied by rise in serum concentration of elements usually excreted by kidney (urea, creatinine, uric acid, organic acids, and the intracellular cations—potassium and magnesium). b.There can be a decrease in renal function with increasing nitrogen retention even when the patient is excreting more than 2 to 3 liters of urine daily—called nonoliguric or high-output renal failure.
4.2.3. l.Diuretic phase: a.Begins when the 24-hour urine volume exceeds 500 mL and ends when the BUN and serum creatinine levels stop rising.
4.2.4. Recovery phase : a.Usually lasts several months to 1 year. b.Probably some scar tissue remains, but the functional loss is not always clinically significant.
