1. Ureteres
1.1. 3 layered tubes
1.1.1. transitioned epithelium and goblet cells
1.1.2. smooth muscle
1.1.3. Areola connective tissue contacting blood vessels, lymphatic vessels and nerves.
1.2. plant into the bladder at a shallow angle.
1.3. Peristalsis moves urine from renal pelvis to the bladder.
2. The Urninal Bladder
2.1. in males it is in front of the rectum and in females it is front of the vajina and below the uterus.
2.2. situated behind the symphysis pubis.
2.3. Folds of peritoneum holds it in place.
2.4. Bladder capacity on average is 700-800ml - smaller in females and over filling can lead to a rupture.
2.5. Lined by transmittal epithelium which can fold as rugae.
2.6. The desirous is 3 layers of smooth muscle.
2.7. The outer superior layer is peritonuem; inferior this is a fibrous covering,
3. Urethra
3.1. In women
3.1.1. is 4cm long
3.1.2. travels slightly curved as passes inferiorly through the pelvis floor into the perineum.
3.2. In men
3.2.1. is 20cm long
3.2.2. bends twice along its course
3.2.3. male bladder is slightly bigger than females - less likely to get urine infections.
3.3. It is the exit tube from the bladder to the outside - the flow of urine is controlled by 2 muscular spincher.
3.3.1. internal uretha sphincter
3.3.1.1. involuntary
3.3.2. external uretha sphinchter
3.3.2.1. voluntary
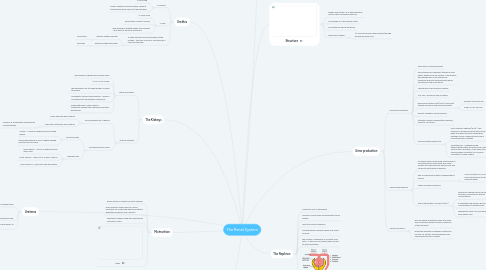
4. The Kidneys
4.1. external anatomy
4.1.1. each kidney is shaped like a kidney bean
4.1.2. 12 x 6 x 3 cm in size
4.1.3. the indentation on its media border is called renal helm
4.1.4. perivepetic fat surrounds kidneys - anchors the kidneys to the posterior abdominal.
4.1.5. underneath lives a renal capsule - connective tissues that shapes and protects the kidneys.
4.2. Internal anatomy
4.2.1. can be divided into 2 regions
4.2.1.1. Outer light red renal capsule
4.2.1.2. inner dark red/brown renal capsule
4.2.1.2.1. contains 8-18 pyramids separated by column/tissues.
4.2.2. functionally has 2 zones
4.2.2.1. functional area
4.2.2.1.1. contex - 1 millions nephrons found in each kidney
4.2.2.1.2. striped appearance is due to tightly packed pactical loops of henle.
4.2.2.2. drainage area
4.2.2.2.1. Renal papilla - 1000's of papillary ducts drain urine.
4.2.2.2.2. Minor calyces - drain into 2-3 major calyces
4.2.2.2.3. major calyces - drains into the renal pelvis.
5. Mictrurition
5.1. Reflex action in infants and small children
5.2. older children/ adults learn to control mictrution by controlling external uretheral sphincter and pelvic floor muscles
5.3. eventually bladder filling with override his voluntary control.
5.4. reflex
6. Normal urine
6.1. volume - 2000ml per 24 hours
6.2. yellow/amber In colour
6.3. clarity - transparent when fresh
6.4. smell - mild aromatic when fresh
6.5. pH should range from 4.6-8.0
6.6. specific gravity - range 1.001 - 1.035
6.7. Normal
6.7.1. water, urea, uric acid, creature and excess inorganic salts
6.8. Abnormal
6.8.1. albumin, glucose, red + white blood cells, ketonic bodies, bilibin, urobilden and bacteria.
7. Structure
7.1. Kidney abd urerers lie in the abdominal cavity; partly covered by the ribs.
7.2. The bladder is in the device cavity.
7.3. The urethea is below the pelvis.
7.4. Renal blood supply
7.4.1. 1/4 of bodys blood supply passes through the kidneys every min.
8. The Nephron
8.1. Functional unit of the kidney
8.2. consists of renal tube and associatcy blood vessels
8.3. most are cortical nephrons
8.4. juxtameduallary nephrons have long loops of henle.
8.5. the number of nephrons is constant from birth - if they are lost, others take on extra to work effectively.
8.6. Structure
9. Urine production
9.1. Glomerular filteration
9.1.1. takes place in the glomerulus
9.1.2. blood pressure in different arteries forcing water, waste and most solutes in the plasma through the wall of the glomerular capillaries and into the glomerular which empties into the renal tubule.
9.1.3. Takes place in the bowman capsule
9.1.4. 150-180 L blood per day is filtered.
9.1.5. glomerular filtration rate (GFR) is the aunt filtered formed by kidneys each minute
9.1.5.1. females 105ml per min
9.1.5.2. males 125 ml. per min
9.1.6. Directly related to blood pressure
9.1.7. filteration ceases if hydrostatic pressure drops to 45 mmHg.
9.1.8. Hormones that effect GFR
9.1.8.1. Arial Natriretic Peptide (ANP) - this hormone is produced by the atria of the heart and when pressure inside them exceeds normal. meaning more fluid is circulating than is healthy.
9.1.8.1.1. the response of the hormone is to squeeze more blood filtrate through the glomerulus so excess fluid will go through the bladder reducing blood pressure.
9.1.8.2. Angiotoenism - released during haemorrhage states will result in too little fluids in the circulation, it will lower GFR and reduce kidney circulation to conserve circulation to other organs.
9.2. Tubular Reabsorption
9.2.1. as filtered fluids move along renal tubule to collecting ducts most water and useful solutes are reabsorbed by tubular cells and retried to pertitubular capillaries
9.2.2. 99% of glomerular filtrate is reabsorbed by tubular
9.2.2.1. occurs mostly in PCT but DCT and collecting ducts can reabsorb water
9.2.3. under hormone influences
9.2.4. The Antidiverative Hormone (ADH)
9.2.4.1. stored and released from the posterior pitvitary in response to plasma concentration
9.2.4.2. it regulates fluid balance by the concentration of diluted urine
9.2.4.3. dehydration rises ADH and excess intake of fluid lowers ADH
9.3. Tubular Secretion
9.3.1. process where substance move into distal and collecting tubules fro blood, mainly by active transport.
9.3.2. important because is disposes substances not real for filtrate, removing excess ions, maximising removal of waste.

